How to treat coordination of movements after a stroke. Stroke loss of coordination After a stroke, movement coordination is impaired what to do
Ataxia after a stroke - symptoms, diagnostic tests, treatment
Ataxia is one of the types of movement disorders that occurs in patients after a stroke. This is a collective concept that includes several types of impaired coordination of movements. In clinical practice, cerebellar ataxia is most common, the cause of which is a violation of blood circulation in the cerebellum. According to statistics, cerebellar stroke is not so common - in about 10% of cases.
However, more than half of the episodes of this type of stroke end in death, and a very high percentage of disability is recorded among the survivors.
Ataxia is a violation of coordination of movements and motor skills.
Classification of ataxias
Normally, coordination of movements is regulated by the following parts of the brain:
- medulla oblongata and midbrain;
- cerebellum;
- vestibular apparatus;
- frontotemporal cortex of the cerebral hemispheres.
In the posterior part of the brainstem are the bundles of Gaulle and Burdach. They are responsible for deep muscle sensitivity. The main task of the cerebellum is to complement and coordinate the work of the motor centers. Thanks to him, the movements become smooth, clear and proportionate. The cerebellar vermis maintains normal muscle tone and balance. Thanks to the coordinated activity of the vestibular nuclei, balance is maintained during movements. The frontal cortex is responsible for voluntary movements.
It is difficult to say which of these departments is the most important in the coordination of movements. All of them are connected by numerous synaptic connections, which ensures normal motor activity. Depending on where the stroke occurred, clinicians distinguish between the following types of motor coordination disorders, or ataxias:
Sensitive ataxia
This type of ataxia develops after a stroke in the posterior columns of the spinal cord, the thalamus. It can appear in both limbs, one arm or one leg. This type of movement disorder is characterized by loss of proprioceptive sensitivity. The patient cannot assess the position of his own body parts. There is a so-called stamping gait - the patient bends his legs excessively and steps very hard on the floor. Often complains of the sensation of walking on soft carpet. The victim constantly looks at his feet, thus trying to alleviate the pathological symptoms. When the eyes are closed, the manifestations of ataxia intensify.
Cerebellar ataxia
Develops after a cerebellar stroke. There is unsteadiness when walking. The patient deviates towards the lesion, in severe cases falls. If the cerebellar vermis is affected, a fall is possible in any direction and backwards. Walking is wobbly, with legs wide apart. Walking with a side step is impossible or sharply impaired. Hand movements are disproportionate, slowed down. The arm and leg on the side of the lesion are most affected. Speech slows down, becomes drawn out, chanted. In contrast to aphasia, where the basis of speech disorders is the death of neurons in the cortical centers, in patients after a cerebellar stroke, coordination of movements is disturbed. The handwriting changes - the letters become sweeping, large.

Distinctive features of the gait of a patient with ataxia
vestibular ataxia
Vestibular ataxia is manifested when moving, sitting or standing. Symptoms are aggravated by turning the head, trunk, eyes. The person refuses to perform these movements, replaces them with others, or performs in slow pace. Thanks to visual control, it is possible to significantly compensate for impaired coordination. With a unilateral lesion of the vestibular nuclei, shakiness and deviations of the body occur in the direction of the lesion. Movement disorders are especially noticeable when walking with closed eyes. Vestibular ataxia is accompanied by severe autonomic disorders - nausea, dizziness, nystagmus.
Cortical ataxia
A specific disorder of coordination of movements that develops in patients after a stroke in the frontal lobe of the cerebral hemispheres. Mostly in such situations, the legs suffer. The hands are not involved. The patient's gait is uncertain, shaky, along one line. The body leans back. The patient cannot stand and walk, despite the fact that he has no signs of paresis or paralysis.

Clinical manifestations of cortical ataxia
Diagnostic tests
Diagnosis of impaired coordination of movements in patients after a stroke is based on the following points:
- patient complaints;
- inspection data;
- diagnostic test results;
- data from the results of additional research methods.
Coordinating tests allow you to determine the type of ataxia, to establish the location of the stroke.
The first is static ataxia. The patient is placed in the Romberg position - legs together, arms forward, eyes closed. The stability of the patient is assessed. After the usual Romberg test, a complicated one is carried out - they are asked to stretch their hands in front of them at shoulder level, spread their fingers to the sides, put their legs so that the toe of one touches the heel of the second limb.

Study of the function of the cerebellum
Then the gait is evaluated. The patient is asked to walk in a normal gait in a straight line, heel to toe and flank gait.
After that, the diagnosis of dynamic ataxia is carried out. The patient is asked to extend his arms in front of him and reach the tip of the nose or the malleus with the index finger. The test is carried out with open and closed eyes.
The symmetry and synchronism of movements can be assessed using an asynergy test - the patient is asked to stretch his arms in front of him and make movements similar to screwing in light bulbs. Another diagnostic test is for dysmetria. The patient needs to raise both hands to shoulder level and stretch them in front of him. After that, you need to raise one hand vertically up and lower it to the level of the second. The test is repeated on the opposite side.
Heel-knee test - in the supine position, the patient should touch the heel of one leg to the opposite knee.
Asinegria Babinsky - the patient is asked to sit down with his arms crossed over his chest. If the cause of impaired coordination of movements is in the cerebellum, it is not the body that rises, but the legs.
Treatment
In patients after a stroke, in the first hours after the disease, the resumption of blood circulation in the focus of necrosis comes to the fore. Then nootropic and vascular agents are prescribed. Their main task is to reduce the size of the focus, to help the surviving neurons integrate into the overall activity of the central nervous system.
As soon as it becomes possible, the patient begins motor gymnastics.
To improve coordination, it is necessary to perform complex purposeful actions - to lift small objects from the floor, to open locks, to “catch up” with moving objects with your hands, to press buttons located at some distance from the patient. If it is necessary to coordinate the movements of two joints, then one of them is fixed and movements are carried out without it.
With vestibular ataxia, exercises are carried out with an increase and decrease in the area of \u200b\u200bsupport, with the elimination of visual control - in the dark, blindfolded, with headphones. It is recommended to walk on uneven terrain, backwards, on a stencil. It is very useful to combine such exercises with gymnastics for the eyes.
An important role is played by massage, passive gymnastics, physiotherapy procedures.
Intensive walking after a stroke

As obvious as it may sound The best way improve the quality of walking is to walk.
Walking can be used in some of the most advanced approaches in modern recovery research. For example, one of the methods used by researchers to encourage rapid recovery is called specialized training. This means training for recovery in the context of a meaningful task. There are tasks that are more valuable than walking. Walking is also related to another popular concept from rehabilitation research: repeated practice(by repeating the same movement). Researchers believe that repetitive practice is important for mastering lost skills. Another cutting-edge approach to stroke rehabilitation is to add a component rhythm. Walking is inherently rhythmic. It is also related to another method of recovery that researchers love - bilateral training, suggesting the stimulation of the interaction of two legs. Researchers believe that the arms and legs are connected to each other in two ways:
- limbs "communicate" through the brain;
- the limbs "communicate" directly, directly through the spinal cord, without the participation of the brain.
Thus, walking combines four modern concepts:
- The significance of the task: involves training exactly what needs to be learned.
- Repetitiveness: involves performing the same movement many times.
- Rhythm: suggests rhythm. Walking itself provides the rhythm.
- Bilateral training: based on the relationship between the two legs. During bilateral training, a healthy limb can make the diseased move better and faster.
Walking may be the best exercise available.
- refers to physical exercises with a low impact load, so it slightly strains the joints;
- helps to store energy for the heart and lungs;
- burns calories and helps control weight;
- helps control blood sugar levels;
- increases mental alertness;
- reduces the likelihood of blood clots in the legs, which reduces the risk of another stroke;
- promotes muscle growth;
- improves balance and may reduce the risk of falling;
- strengthens bones;
- . brings many other benefits.
How it's done?
There are many ways to keep yourself safe while doing brisk walking. You can discuss with your doctor and physiotherapist the use of suitable orthopedic appliances such as orthopedic device "ankle-foot" (OASL), and related walking aids, in particular canes and walkers. However, if you are not yet ready to walk without support, there are other options (other than wearing a belt that two therapists hold you by as you walk). All of the following should be done under the supervision of a physiotherapist.
Treadmill workouts (TBD). They can provide safety and comfort when walking indoors using "infinite parallel bars". But running on a treadmill comes with a risk of falling.
Walking with Partial Body Support (CPBT).
- HFPT on a treadmill: You are partially supported by straps. The straps can be pulled up to reduce the weight you're carrying, or lowered so you can carry your full weight, but the straps keep you safe if you fall. This allows you to train your sense of balance without the risk of falls. The simulator commonly used in this type of training is called LiteGait.
- HCPT by flat surface: This system is the same as the treadmill version, except that you are walking on a level surface. Machines that fall into this category include the Biodex Unweighing System, the NeuroGym Bungee Walker, and the LiteGait. Contact a physical therapist or local rehab clinic to find equipment in your area that provides CPPT.
The researchers got good results using a new type of walking recovery - interval training on a treadmill. The idea behind this method is simple: your walking will get better and faster if you practice walking faster. Brisk walking improves the quick movements needed for balance control, resulting in smoother, more efficient walking. Interval training on a treadmill were used to double the walking speed of study participants.
What precautions should be taken?
Walking is one of the most natural types of movement performed by humans, but a walking regimen designed to improve gait quality requires more physical and mental effort than normal walking. Because this walking regimen is more intense than normal walking, talk to your doctor and therapist before incorporating therapeutic walking into your overall recovery plan. If you can walk on your own, do so safely. Your doctor and therapist will talk to you about the medical and physical restrictions you need to follow.
How to learn to walk after a stroke
Recovery of walking after a stroke occurs in stages. The muscles of the legs and torso are strengthened gradually, the ability to coordinate their movements and maintain balance returns. It takes a long time to eliminate movement disorders, but if you make an effort, you can achieve good results.
Implications for motor function
With a stroke, there is an acute violation of blood circulation in the brain. As a result, the body suffers from a lack of oxygen and nutrients, which leads to cell death. After an attack, the following disorders occur:
- The ability to walk is impaired. The patient cannot get out of bed on his own.
- There are sharp mood swings, positive emotions are replaced by negative ones.
- Cognitive functions become unstable.
- There is no connected speech.
- There is a violation of swallowing reflexes.
In the presence of these disorders, treatment should be started as soon as possible, otherwise complete paralysis will occur.
Not a single specialist can say exactly when a person will fully recover from an attack. The rehabilitation program is selected separately for each case. This also applies to the development of exercises to restore the ability to move.
After an acute circulatory disorder in the brain, motor function disorders can be detected by the following signs:
- Unsteadiness of gait appears, which is not observed in healthy people.
- Unable to bend and straighten the leg and arm or fully straighten. The leg can always remain in a straightened position.
- The gait becomes uncertain, and the steps are wrong. Unable to move quickly.
- It is not possible to fully stand on the sole of the injured leg. Therefore, the patient begins to walk from the toe, and not from the heel, as ordinary people do.
- Each next step can lead to an unexpected drop, as sensitivity decreases.
- The movement of a sick person resembles a compass.
Some patients recover very quickly and learn to walk within 2-3 months after the attack, while others need much more time. It all depends not only on the degree of lesions, but also on the correctness and regularity of home treatment. The use of special simulators speeds up the recovery process, but not everyone can afford it. Therefore, many use homemade devices for training leg and arm movements.

If after a stroke the legs do not go well, what to do, you need to find out from the experts. The rehabilitation period should begin as early as possible, but only after the completion of drug treatment.
First, the patient must learn to sit, and only then can he try to get out of bed. At first, even sitting will be difficult, so relatives should make sure that the patient does not fall.
Gradually, the victim will begin to maintain balance, be able to keep the torso in correct position what is needed for walking.
You should also restore the ability to bend and unbend the leg and arm.
Recovery is facilitated by the use of:
- special cane with four supports;
- orthopedic shoes with a small heel and a wide sole. It is desirable that the fasteners fix the ankle joint of the affected limb well.
It is necessary to ensure that a person after a stroke develops independence in himself and is able to serve himself and walk without outside help.
How to develop a gait
In order for the patient to be able to learn to walk after a stroke, he needs help. In rehabilitation centers, the technique of drawing a path with traces in front of the bed is used. On them, patients begin to take their first steps. This method can also be used at home. It helps you recover faster motor functions.
It will be easier for the victim to start walking after a stroke if:
- use holders to fix the foot;
- wear knee braces so that the knee does not bend and the leg is held in a vertical position.
After the ability to rise to its feet without assistance has returned, you can connect treadmill designed specifically for stroke patients.
It is important that the classes are not carried out at a fast pace, as the ankle joint may not work correctly.
Recovery speed can be different:
- If a stroke manifested itself in the form of a small ischemic circulatory disorder, then the ability to control the limbs to a person will return within a month.
- The average degree of a stroke, which is always accompanied by a loss of consciousness, allows only half to maintain motor activity. Therefore, the patient must be gradually taught movements. First, it will be enough to warm up in a prone position. Gradually, you should move on to more complex exercises.
- A stroke, accompanied by severe hemorrhage, leaves no chance of recovery. This condition is considered incompatible with life.
The order of training
Recovery of limbs after a stroke consists of:
- passive gymnastic exercises in bed;
- sitting in bed;
- getting up and standing still without support;
- walking with the use of technical means of rehabilitation, and later without them.

Restoration of the vestibular apparatus after a stroke is very important, since with its help a person keeps balance. All training should be carried out, gradually increasing the load. It is impossible to start teaching the patient to walk if he still cannot sit up in bed on his own or make even the simplest movements.
Exercises for the legs after a stroke are developed individually. They should be as physical as possible.
You need to master the exercises in this order:
- The first group consists of turning from side to side in bed, pushing the body with the legs from the headboard, trying to take a sitting position and lying down without falling.
- The second group reinforces the ability to sit independently. During this period, you can do active gymnastics while sitting, lower your legs from the bed and get up on a healthy leg.
- The third group can be started when the patient is stable on a healthy leg. In this case, you can already use a walker.
- The fourth group - with the help of a walker, you can stand and carefully step from foot to foot.
- Those who have passed to the fifth group can independently develop a stable gait using walkers. The legs can already withstand heavy loads, the patient can walk more distances than before, the intensity of the exercises can be increased.
In theory, this option is considered ideal. But in practice, everything is much longer and more difficult. Failures often occur, there are breaks in progress, there are bouts of depression and loss of faith in one's own strength. But gradually faith in victory returns, and the treatment continues.
How to learn to use a walker
As soon as the patient learns to stand confidently on his feet without support, he can begin to take his first steps. You cannot do without an assistant in this matter, since he must belay from the paralyzed side in order to prevent a fall.
The patient should put his hand on the assistant's neck and rest his knee on his knee. Having fixed the joint, you can take the first step.
The task of the assistant is not only to support the patient, but also to control the correctness of his gait. When the patient moves with the help of a walker, it is necessary to ensure that the position of the foot, the turn of the knee and the hip joint are correct.
The whole process has several features:
- The patient cannot fully grasp the assistant with his hand, as it is weakened.
- To take a step, he needs to throw his leg forward, which leads to clinging to the helper's leg.
- It is much more convenient to support the patient from a healthy part of the body, but the knee joint will not be fixed and the patient will not be able to hold on to the wall with a healthy hand.
The main purpose of using a walker is to gain the ability to bend the leg in all joints, otherwise the patient will constantly cling to the floor with the foot. The assistant should remind the person that the leg should be raised higher and bent at all joints.
High boots that fix the ankle joint will help facilitate movement. The sore arm should be fixed with a scarf so that during movement it does not sag, and the head of the shoulder does not come out of the articular cavity. During classes, you should control the work of the patient's heart and give him rest.
When the patient learns to move with the help of a walker without assistance, it is possible to start walking independently. This is done with a cane, holding on to the walls, moving a chair in front of you. But it is important to ensure that the load is evenly distributed. It is impossible to spare a sick leg, relying more on a healthy one.
Massage treatment
Massage can be used to speed up the healing process and improve blood circulation in the brain. Foot massage after a stroke (and the whole body) is performed using:
- Stroking. With a relaxed palm, they glide over the surface of the skin, collecting it into large folds. At first, stroking should be superficial, but gradually their depth should be increased. They must capture adipose tissue and muscles. The hand of a specialist should move in zigzags, a spiral. With the help of this massage, you can bring the body into tone and, by removing the top layer of cells, improve blood circulation and tissue nutrition.
- Rubbing. This increases the elasticity of tissues, reduces swelling due to the movement of fluid. You need to rub the skin with the help of fingertips, the base of the palm or a hand clenched into a fist.
- Kneading. This is a kind of passive gymnastics. During the procedure, the muscle is captured, pulled and squeezed. There is also some effect on the vessels. Kneading helps to increase the elasticity and tone of muscle fibers. Therefore, in the presence of spastic changes, the procedure is prohibited.
- Vibrations. The specialist performs oscillatory movements with a relaxed hand on the affected part of the patient's body. Massage with different speed and amplitude. Therefore, the result may be different. If the vibration is strong, then the muscle tone decreases, and if it is high, it increases. Movements are usually performed from right to left.
Similar treatment can be carried out at home. It is carried out independently by close people, hire a specialist or use massagers.

Relatives of the victim should perform massage from the side of the lesion, gradually moving to other areas. After a stroke, people remain in good shape only:
- palmar surface, front of the shoulder and forearm;
- chest muscle;
- front surface of the thigh and back of the leg;
- sole muscles.
These areas can only be massaged superficially by stroking or lightly rubbing. For other areas, heavy traffic is suitable.
When massaging the patient in a supine position, you need to put a pillow under the head, and a roller under the knee. To prevent a healthy limb from moving, it can be fixed with weights.
The recovery process after a stroke is difficult and lengthy, but if the victim himself and his relatives make every possible effort, the result will be positive.
How to help regain walking after a stroke?
Hello. I decided to write something important about the restoration of walking after a stroke. The help of only professionals and specialists in this matter is not always needed, sometimes relatives and those who are nearby can provide important and feasible assistance. The main thing is the desire to help.
Rehabilitation in this case is a multifaceted process and it is necessary to take into account all the factors that can contribute to recovery - from the patient's internal mood to clothes and shoes, which can greatly facilitate and help to take new independent steps.
I want to talk in this article about shoes that can help a lot with walking training. Let's talk about what these shoes should be like and what to pay close attention to when choosing them. The topic is important and relevant.
Violation of walking after a stroke: the essence and ways of solving the problem.
Before we move on to the selection of shoes, a small introduction, let's figure out what the salt of walking disorders after a stroke is. Loss of mobility and muscle strength, as a result of which a person loses the habitual ability to move independently, is a frequent phenomenon after a stroke. Most often, walking disorders occur with hemiparesis.
Restoring habitual mobility is a complex process, which should include not only pills, injections, etc. - everything that is called drug therapy, but also other recovery methods, including adaptation to environmental conditions. These adaptation methods may make a greater contribution to the restoration of proper walking after a stroke.
Although it is not always possible to recover from any neurological disorder, one of the main goals of recovery after a stroke is to make a person independent in everyday life, as much as possible.
In most cases of post-stroke hemiparesis, there is an increase in muscle tone in the ankle extensors.
 Fig. 1 Wernicke-Mann gait
Fig. 1 Wernicke-Mann gait
Outwardly, this position looks like a person is pulling a toe, while the foot is slightly turned inward. Such a foot is unstable when walking, as a result of the fact that it can cling to the surface or tuck when a person takes a step. In addition to the fact that it is simply uncomfortable to walk and independent walking becomes difficult, the very restoration of walking is seriously hampered. The physiological step, in this case, is very difficult.
How more people makes movements that are as close as possible to a normal gait, the faster it (the gait, in the sense) will recover. This works with an important condition - the biomechanics of the step should be as close as possible to the physiological (not pathological) step. To do this, you need to support the foot more and more often in a physiological position (from extended to half-bent).
Properly selected orthosis and / or shoes will help us with this. The topic of choosing an orthosis deserves a separate article, and I will definitely tell you about it in more detail.
In this article, we will discuss shoes with which we will solve the problem of stabilizing the ankle joint and placing the foot in a position as close as possible to the physiological and necessary for proper walking.
How to choose the right shoes for hemiparesis. Which
need shoes?
We will analyze the main requirements for this shoe and I will also show you with a couple of examples - what such shoes look like and where to find them.
footwear requirements.
- Shoes must close to the surface of the body, well fix and keep the leg in the desired position.
If the shoes are loose on the foot, it will make the steps unstable and wobbly, which increases the risk of falls and injury. - These shoes must be easy to put on, take off and fix even with one hand. With hemiparesis, strength is reduced not only in the leg, but also in the arm. Sometimes, the movements in her are completely lost and she cannot help put on shoes with a healthy hand. You need shoes that can be put on and taken off with one hand, and also fixed with one hand. The lace fastening is not quite suitable, although it has a large plus - good tight fit on the leg. This disadvantage is the difficulty in lacing - this requires two working hands. With hemiparesis, often, there are motor disorders in the hand. A suitable option is shoes with fixing straps on a sticky strap.
- This shoe shouldn't be too heavy.
Fixation of the ankle joint will be performed by shoes with a high back. That is, these are shoes with a high grip on the area above the ankles. This shape of the shoe makes the ankle joint more stable. It dangles less when walking, the sock during the step clings to the surface less.
 Fig.2. With a high grip on the ankles.
Fig.2. With a high grip on the ankles.
An example of such shoes is in Figure 2.
Of course, shoes should be suitable for the season, so that it is comfortable in it - not cold and not hot. It may differ in purpose - for kinesiotherapy (physiotherapy exercises) to restore walking. Or for everyday use - walking on the street, for example.
 Sports shoes with a high grip on the ankles.
Sports shoes with a high grip on the ankles.
- So, option one. Shoes for everyday use and walking on the street in the off-season and summer. These are high heel sneakers, while they are soft and light, they fix the ankle joint well. During hot weather, it is possible to wear sandals with the same good fixation of the ankle.
- Option two, it's winter shoes. Again, when choosing winter shoes, we are guided by the above requirements, as well as for shoes of other seasons. In fact, such shoes can be seen quite often on the winter streets (lightweight fabric boots with a sticky closure). You can generally find it.
- Option three. These are shoes that can be worn when walking is restored. Such shoes are always needed and in demand - this is what you can wear in the hall of physiotherapy exercises, that is, indoors. Again, you can also choose an option from sports shoes. In addition to the same requirements, keep in mind that the sole of such shoes should not be too soft - like "Czechs" or "ballet flats". The soft fabric sole can easily cause dangerous slips and fall threats. You need a solid, stable sole - not necessarily a thick one.
With the individual selection of such shoes, the main condition is the obligatory fitting and its “testing” on the spot. Such shoes should not only sit comfortably, but also securely hold the ankle itself, and also be stable on the surface when the center of gravity moves to this leg. Usually, when you first get acquainted with the shoes themselves, this is felt and it is noticeable.
A lot of people have a problem with the search and selection of such shoes. In specialized stores of medical equipment, from what can be used for spastic hemiparesis, there are only orthoses. Finding shoes suitable for hemiparesis is not always easy - even if you know exactly what kind of shoes you need and what to look for when looking for them. Sometimes, loved ones bend down to find her and do not always find a suitable option.
When choosing a purchase, a suitable option may be to search for suitable shoes first by someone close and the possibility of trying on and returning if they do not fit.
Be careful with your choice of shoes. Ultimately, such shoes are a reliable assistant in restoring walking, and this is the main step towards regaining independence and successful rehabilitation in general. Thank you for your attention!
Rehabilitation after a stroke: how to learn to walk
A stroke claims millions of lives around the world, leaves people disabled, and not everyone is able to fully recover from an attack. The consequences of a blow can be complete or partial paralysis, loss of habitual skills, a person becomes incapacitated and requires regular self-care from the outside. Dependence of the patient on caregivers along with the state of health provokes psychological problems. In this case, the help of a psychologist is required, the patient must be prepared for difficulties on the way to recovery.
 Restoration of motor functions is an important stage of rehabilitation.
Restoration of motor functions is an important stage of rehabilitation.
In addition to supporting close people, the patient himself must make considerable efforts to restore lost functions. The rehabilitation period can last from several months to years. The course consists in the use of complex measures aimed at restoring speech, motor, cognitive functions. When the crisis period has passed, the patient needs a long rehabilitation, because learning to walk again after a stroke can be very difficult. Rehabilitation measures should not be delayed, they should be started immediately after drug therapy to restore cerebral circulation. The patient should not get used to bed rest, the sooner he can get out of bed, the faster the recovery process will start.
Impact of stroke on motor functions
Acute circulatory disorders cause failures of all body systems. In addition to incoherent speech, dysphagia, the patient has numbness of the limbs, paralysis. If time does not take action, these symptoms can flow into a permanent phenomenon. The presence of muscle cramps can be extremely dangerous and herald a recurrence of an attack.
The following signs are characteristic of impaired motor functions:
- there is uncertainty, unsteadiness of gait;
- inability to develop speed of movement;
- the patient cannot bend, straighten or straighten the arm or leg as much as possible;
- painful spasm of the muscles of the legs prevents flexion of the pelvic and knee joints, often occurs in the foot;
- movements of the paralyzed leg may exacerbate arm spasms;
- coordination of movements is broken;
- partial or complete lack of sensitivity of the limbs;
- the patient cannot put his foot on the sole, as a result, when walking, the movements begin with the toe, and not with the heel;
- walking after a stroke can be accompanied by sudden falls.

Rehabilitation measures begin to be carried out on an individual basis, there are no clearly established deadlines for the recovery process, it all depends on the patient's condition. Some patients begin to walk after 2 - 3 months, others need much more time to return the lost functions. In any case, the patient and loved ones need to be patient and work to get a positive result.
Despite the significant influence of the extent of brain damage on the dynamics of recovery, the support of relatives renders a great contribution to the success of the measures. No less important is the psychological attitude of the patient himself. A depressive state caused by a feeling of helplessness, doom and unwillingness to act can ruin all the ongoing rehabilitation work in the bud.
Drug therapy does not end after the acute phase of the pathology. The patient may be prescribed medication for a long period, depending on the condition and symptoms:
- drugs that stabilize normal blood flow through the vessels, normalize the work of the heart;
- means for lowering blood pressure in case of its high rates;
- blood thinning drugs that prevent the formation of blood clots in the extremities (not used for hemorrhagic stroke);
- muscle relaxants that relieve muscle spasms;
- neurotrophic drugs that promote motor activity;
- antioxidants to restore brain cells.

How to start walking after a stroke
To get a person out of bed as soon as possible, you need to start with simple exercises, gradually moving on to more serious training. A patient after a stroke is extremely unmotivated and often does not want to do anything to improve his condition. The task of the psychologist and close people is to positively set the patient up for recovery. Despite the length of the rehabilitation period, the patient has a chance to regain all or part of the functions lost as a result of an attack.
Recovery procedures include the following:
- At the first stage, passive charging is required, which does not require getting out of bed. It is carried out by health workers or relatives of the patient. Gymnastics trains the function of flexion of the joints, for this they alternately raise, bend one or the other arm at the elbow, then carry out similar exercises on each leg.
- The simulator bed is designed to start the process of learning the correct movement of legs on initial stage, it mimics walking.
- Approximately 4-5 days after the attack, the patient is trying to sit down. A special device helps to achieve a vertical position. First, the patient sits on the bed, then hangs his legs on the floor.
- Further, you can imitate walking by moving your legs in a sitting position. The need for an upright position is not established by exact terms and depends on the individual condition of the patient.
- At this stage, preparatory work is underway for the practice of walking, it is effective to use the “bike” movement, since it involves all muscle groups.
- Hydrotherapy, which involves the use of hydromassage, improves blood circulation.
- Ozokerite applications, treatment with paraffin compresses.
- Massages are an effective and integral part of the treatment.
- Hydrotherapy, ozocerite applications, massages help to get rid of muscle cramps.
- Rehabilitation is successfully carried out at home, where the patient tries to perform ordinary household activities that develop motor skills.
- The use of simulators significantly speeds up the recovery process. There are several types of devices for developing walking skills, getting up from a chair, exercise bikes, treadmills.
- After some time (the rehabilitation period is individual), the patient manages to get on his feet. Standing and walking are not easy for a patient in a post-stroke state. You should start taking the first steps with the support of another person, then independently with the help of supports.
- You can mark the traces of the patient in order to further correct the gait. To consolidate the skill of correct foot placement, you need to walk along a marked path with steps specially marked on it.

With the beginning of the stage of learning the skill of walking, it will be necessary to acquire:
- orthopedic shoes with wide soles with a slight rise;
- special holders are used to fix the foot;
- It is also advisable to wear knee braces so that the leg does not bend at the knee while walking.
Often, after a stroke, the legs do not go well, what to do in this case, they know in the rehabilitation center, but not everyone has the opportunity to afford expensive procedures. No less effective can be home walking training according to the principle “I will teach you to walk the way I walk myself”, exercises can be done with the help of loved ones.
Walking Exercises
The number of repetitions will depend on the condition of the patient, if some exercises are beyond his power, the patient can be helped. Too much active exercise best done when the patient feels better.
- in the supine position bent legs at the knees, the patient straightens one or the other leg, starting with a healthy limb;
- throwing one leg to the other in turn;
- the patient turns the feet inward, then to the sides;
- extension and flexion of the joints of the arms and legs;
- exercise "bicycle";
- abduction of the leg to the side: the exercise is performed lying on your back with legs straightened or bent at the knees;
- lifting the pelvis: the legs are bent at the knees, in the supine position the patient raises and lowers the pelvis;
- transfer of a straightened leg over the other;
- flexion of the legs;
- lying on his side, the patient should raise and lower his leg, then, turning over to the second side, do the same with the second leg.
It is not so easy to regain muscle control, but the efforts made by the patient and his family sometimes achieve incredible results. In medical practice, there are many cases when, it would seem, completely hopeless patients returned to their former lives.
Walking after a stroke
Movement disorders are the most common complications of stroke. They are observed in more than 80% of patients. Of these, only 20% are fully restored. The effectiveness of rehabilitation depends on the timeliness of medical care at the onset of a stroke, as well as on how early rehabilitation treatment began. The most effective it will be the first six months after a stroke and the completion of intensive care.
Why is walking impaired?
During an ischemic stroke, areas of the brain responsible for motor functions remain without nutrition. These are sections of the pyramidal system, with the help of which a person makes conscious (voluntary) movements. Depending on the site of ischemia and the degree of damage, complete paralysis or paresis of certain muscles develops.
Special brain cells generate impulses to start movement, which are conducted to the muscles using a complex system of neurons. When some of them are turned off from the process, the muscle does not receive commands "from above" and remains motionless. At the same time, all possible motor programs are stored in the "card file" of the lower motor system.
The task of motor rehabilitation is to restore the lost connections between the brain and muscles, help the body "remember" the necessary motor programs and restore the brain's ability to control them.

With it to start recovery?
The first thing done after a stroke to prevent loss of motion in the joints and tendons is treatment with position. To do this, the leg is fixed in a straightened position with a slight turn inward and the foot resting on the headboard. Fixation is carried out within 1.5 - 2 hours.
Passive exercise
Recovery of walking after a stroke begins with training individual muscles and joints. A stroke usually affects one hemisphere of the brain. In this case, they speak of hemiparesis or hemiparalysis - a unilateral impairment of motor functions. Restoration of movements in a sore leg begins with passive exercises.
They are performed by an exercise therapy specialist, gradually including the patient himself in the process, that is, gradually transferring passive movements into active (controlled) ones. The set of exercises includes:
- flexion, extension and rotation of the feet;
- flexion and extension of the knee;
- flexion, extension and abduction at the hip joint.
If the patient understands well what is required of him, his consciousness must be involved in the process. He must learn to send an impulse to an immobile muscle. To do this, the exercise is done independently with a healthy leg, and then the movement is mentally transferred to the sore leg. The use of muscle memory is perhaps the most important component of the entire rehabilitation process.

Translation of movements into the active phase
The mental message should not fit only in the time allotted for gymnastics. A person striving for a speedy recovery and gaining lost skills should practice throughout the day with short breaks for food, toilet, procedures and sleep.
As the muscle regains strength through passive exercise, the patient must be encouraged to move independently. The assistant sets the amplitude of the movement, and the patient himself must perform it. The movement should be slow and done in parts.
Walking after a stroke is restored with the following exercises:
- Flexion and extension of the legs at the knees. At the same time, the feet slide on the bed. It is performed alternately with the diseased and healthy leg.
- Switching legs. Legs bent at the knees, feet resting on the bed. A healthy leg should be thrown over a sick one, and then vice versa.
- A similar exercise, only one leg should be put on the knee, moving it to the side, then repeat the exercise with the second leg.
- Bicycle exercise.
- Stop turns. Legs are bent at the knees, feet are on the bed. Turning the feet out and in.
- Lying with straightened legs, alternately run the heel of one leg along the front of the lower leg of the other.
- Raising and abducting the legs of the side.
- Raise the pelvis, lying with bent knees.
- Lying on your stomach, bend and unbend your knees.
- Lying on your side, raise your leg.
- Side Turns (restores the skill of turning over in bed). Lying on your back, lower your bent knees to the side, then complete the turn with your torso.

All exercises begin with a healthy leg. You should not immediately ask many approaches to perform one exercise. The number of repetitions depends on the condition of the patient and is increased with great care.
Transfer to a sitting position
A great achievement is the ability of the patient to sit on the bed independently, and most importantly, to maintain this position. Move it to a vertical position gradually and carefully to avoid dizziness and pressure buildup.
After mastering the skill of turning over the patient lying on his side, you need to slowly seat him - the legs are lowered from the bed, the healthy hand is repelled from it. His feet should be resting on the floor and slightly apart, the body is slightly tilted forward to maintain balance.
getting up
The next step is getting up. For training, several exercises are used:
- lifting on the bed - first with the help of an instructor, then - a gradual transition to independent lifting;
- moving along the edge of the bed from back to back - moving the legs on the floor and moving the patient away from the fulcrum of the legs so that he pulls them up on his own.
After lengthy training, the muscles and consciousness of the patient are already ready to get up and hold the body in an upright position. It is important to ensure his safety, as a fall can be frightening and make the patient refuse the next attempt for a long time. Getting up should take place with additional support and the help of an outsider. Trainings are accompanied by explanations of how certain movements are performed correctly. The patient will mentally remember them, stimulating the brain to send impulses.

Before the patient takes the first steps, standing skills are reinforced with exercises:
- Trampling is the transfer of the center of gravity from one foot to another, as if a person is shifting from foot to foot. First, the exercise is performed without lifting the feet off the floor, then they need to be slightly raised.
- Rolling from toe to heel.
- Stepping over an obstacle - at first it can be a pencil, then the height is increased. When performing, the knee should rise high. Steps are taken forward and backward.
- Leading the legs back (the leg is placed on the toe).
Walking recovery
The assistant helps his ward, supporting him from the healthy side. He, as it were, makes a jerky movement, prompting the patient to rearrange the sore leg, and then lean on it.
If it is difficult for one person to cope with learning to walk a post-stroke patient, the help of another person will be needed to rearrange the patient's diseased leg. This happens when the patient is not quite adequate or has a lot of weight.
It is good to alternate daily walking training with exercises on the carpet:
- turning from side to side;
- rolling from one edge of the carpet to the other;
- head lifts;
- getting up on all fours and moving in this position;
- plastunsky crawling.
For these exercises, the instructor will also need an assistant.
Massage to restore walking
It is difficult to overestimate the role of massage in restoring all body functions after a stroke. This is especially true for motor injuries. An experienced massage therapist does not use certain strictly limited techniques. He always proceeds from their condition of the patient and finds by experience an individual way of massage.
Not only a paralyzed leg or arm is subjected to massage. The entire damaged side of the body is massaged, starting from the scalp, ending with the toes. The procedure effectively restores blood circulation in numb skin and muscles, as well as the sensitivity of nerve endings. Massage courses begin 3-4 days after the stroke and should continue for the next year or even two years. Ordinary manual massage successfully complement the hydromassage and underwater shower.
How to ensure safety when restoring walking?
Falling after a stroke can lead to injury. Most often, such patients break the hip of the diseased leg. The reasons may lie not only in the lack of stability of the patient, but also in the imperfection of the environment. It can be slippery floors, too long pile carpets, poorly installed handrails in the bathroom and toilet, and simply insufficient supervision of a sick person.
At the initial stage, when the patient does not feel very confident, special devices will help - a three- or four-point crutch, a walker. To avoid back deflection knee joint an orthosis is used to fix the knee in the desired position.
Usually aids prescribed by the attending physician. He will also determine the deadlines for waiving them. Some fixtures are worth using all the time, for example, handrails in the bathroom.
How long will recovery take?
The possibility of rehabilitation of walking after a stroke and the recovery time depend on many factors - the initial severity of a motor defect (for example, paralysis in the acute stage of a stroke), increased muscle spasm or, on the contrary, their hypotrophy, concomitant musculo-articular disorders.
Significantly inhibits the recovery of cognitive impairment, decreased mental activity, loss of interest in life and depressive states. And vice versa, a well-timed and regularly carried out complex of rehabilitation measures significantly accelerates the restoration of lost functions. Specific terms of the recovery period are individual.
Why is walking important for overall recovery after a stroke?
Having regained the ability to walk independently, the person is ready for further social rehabilitation. Next, a gradual restoration of the ability of self-service, and then household skills, is carried out.
Restoration of movement gives impetus to the restoration of other body functions. The successes that the patient makes and which must necessarily be emphasized by the people surrounding the "stroke", contribute to the restoration of the psycho-emotional state. And this, in turn, gives an incentive to strong-willed efforts, without which full-fledged rehabilitation is simply impossible.
I'm sure you always pay attention to beautiful figure, nice walk. Have you ever wondered what exactly provides our beautiful gait?
Central nervous system: cerebral cortex, extrapyramidal and pyramidal systems, brain stem, spinal cord, peripheral nerves, cerebellum, eyes, vestibular apparatus of the inner ear and of course the structures that all this controls - the skeleton, bones, joints, muscles. Healthy listed structures, correct posture, smoothness and symmetry of movements provide a normal gait.
Gait is formed from childhood. congenital dislocations hip joints or joint can subsequently lead to limb shortening and gait disturbance. Hereditary, degenerative, infectious diseases nervous system, manifested by muscle pathology, impaired tone (hypertonicity, hypotonicity, dystonia), paresis, hyperkinesis will also lead to impaired gait - cerebral palsy. myopathy. myotonia, Friedreich's disease, Strümpel's disease, Huntington's chorea, poliomyelitis.


Gait disorders in myopathies
Properly selected shoes will influence the formation of the correct gait. With tight shoes, the child will tighten his toes, the formation of the arch of the foot will be disturbed, the joints may be deformed, resulting in arthrosis of the joints and impaired gait. Flat feet, clubfoot impair gait. Improper prolonged sitting at the table will lead to curvature of the spine (scoliosis) and impaired gait.

With proper walking, the torso should lean back slightly. The back must be kept straight chest- straightened, buttocks tightened. With each step, the feet should be in line with the toes turned outward. Keep your head slightly elevated. Look straight ahead or slightly up.
Damage to the peripheral nerves - the peroneal and tibial - will lead to impaired gait. “Stepage” - when walking, the foot “slaps”, because dorsiflexion (flexion) is impossible and the foot hangs down. When walking, a patient with a lesion of the peroneal nerve tries to raise his leg higher (so as not to cling to the floor with his fingers), the foot hangs down, when lowering the leg resting on the heel, the foot slaps on the floor. Another such gait is called "cock". The peroneal nerve is affected in compression-ischemic, traumatic, toxic neuropathies. Compression - this means that you have compressed a nerve and / or blood vessels and ischemia has developed - circulatory failure. This is possible, for example, with prolonged sitting. "squatting" - repair, garden; in small buses on long journeys. Sports activities, very sound sleep in an awkward position, tight bandages, plaster splints can cause circulatory disorders in the nerves.

Hanging foot with damage to the peroneal nerve
Damage to the tibial nerve makes it impossible to plantar flex the foot and toes and turn the foot inwards. At the same time, the patient cannot stand on the heel, the arch of the foot deepens, a "horse" foot is formed.

"Horse" foot with damage to the tibial nerve
Atactic gait- the patient walks with legs wide apart, deviating to the sides (often towards the affected hemisphere), as if balancing on an unstable deck, the movements of the arms and legs are not coordinated. Turning the body is difficult. This is a "drunken walk". The appearance of an atactic gait may indicate a violation of the vestibular apparatus, a violation of blood circulation in the vertebro-basilar basin of the brain, and problems in the cerebellum. Vascular diseases, intoxication, brain tumors can be manifested by atactic gait and even frequent falls.
Antalgic gait- with radicular pain syndromes of osteochondrosis, the patient walks, curving the spine (scoliosis appears), reducing the load on the diseased spine and thereby the severity of pain. With pain in the joints, the patient spares them, adapting the gait to reduce the pain syndrome - lameness appears, and with coxarthrosis, a specific "duck" gait - the patient rolls from foot to foot like a duck.
With damage to the extrapyramidal systems. develops in Parkinsonism akinetic-rigid syndrome- movements are constrained, muscle tone is increased, concordance of movements is impaired, the patient walks, bending over, tilting his head forward, bending his arms at the elbow joints, taking small steps, slowly "shuffling" on the floor. It is difficult for the patient to start moving, "disperse" and stop. When stopped, it continues for some time an unstable movement forward or to the side.

Gait of a patient with Parkinsonism
When chorea develops hyperkinetic-hypotonic syndrome with violent movements in the muscles of the trunk and limbs and periods of muscle weakness (hypotension). The patient walks, as if with a "dancing" gait (Huntington's Chorea, St. Vitus's dance).
When the pyramidal system is damaged in various diseases of the nervous system, paresis and paralysis of the limbs. So, after a stroke with hemiparesis, a characteristic Wernicke-Mann posture is formed: the paralyzed arm is brought to the body, bent in elbow joint and radiocarpal, the fingers are bent, the paralyzed leg is maximally extended in the hip, knee, ankle joints. When walking, the impression of an "elongated" leg is created. The patient, in order not to touch the floor with his toe, describes a semicircle with his foot - such a gait is called "circumducting". In milder cases, the patient limps, in the affected limb muscle tone increased and therefore flexion in the joints when walking is performed in a smaller volume.

Gait with central hemiparesis
Some diseases of the nervous system can develop lower paraparesis- Weakness in both legs. For example, with multiple sclerosis. myelopathies, polyneuropathies (diabetic, alcoholic), Strümpel's disease. With these diseases, gait is also disturbed.
heavy gait- with swelling of the legs. varicose veins veins, circulatory disorders in the legs - a person stomps heavily, raising his burning legs with difficulty.
Gait disturbances are always a symptom of some disease. Even a common cold and asthenia changes gait. A lack of vitamin B12 can cause numbness in the legs and disturb the gait.
Which doctor to contact for gait disorders
For any violation of gait, you need to consult a doctor - a neurologist, traumatologist, therapist, otolaryngologist, ophthalmologist, angiosurgeon. It is necessary to be examined and treated for the underlying disease that caused the gait disturbance or to correct the lifestyle, the habit of sitting at the table “foot to foot”, to diversify a sedentary lifestyle with activities physical education, visiting the pool, fitness classes, water aerobics, walking. Useful courses of multivitamins of group B, massage.
Consultation of a doctor on the topic of gait disorders:
Question: how to sit at the computer correctly so that spinal scoliosis does not develop?
Transfer About the most important watch online channel Russia
Signs of a stroke
Stroke is a common cause of death worldwide. Many do not have time to understand what is happening to them, man fail to help. but we will show you how to determine are you at risk of a stroke a few hours, days or weeks before its onset.
Take this simple test help you save your life or the life of a loved one. In the family of our heroine there were strokes, woman fears she is at risk of a stroke. The first sign of an impending stroke is sharp darkening in the eyes.
Then vision can be restored, the balance is lost. Arises  This as a result of a short-term violation of cerebral circulation. Another symptom of a stroke is wobbly gait.
This as a result of a short-term violation of cerebral circulation. Another symptom of a stroke is wobbly gait.
A person's gait is disturbed some time before the stroke. A person often grabs the walls. Take the balance test. For this you need walk straight along the line. Do you have noise in ears, like you put a sea shell to your ear. Some believe that the neighbors are constantly making noise.
Another symptom is this jumps in blood pressure. If the pressure is elevated, then the risk of stroke is high. Vessels are constantly expanding they can not withstand the pressure and burst. When such signs appear need to see a cardiologist. as well as a neurologist who will prescribe vascular drugs.
We remind you that the synopsis is only a brief summary of information on this topic from a specific program, the full video release can be viewed here About the most important issue 766 of May 23, 2013
Was the information useful and interesting for you? Share the link to the site http://osglavnom.ru with your friends on your blog, website or forum where you communicate. Thank you.
Types of walking disorders. Varieties of walking disorders.
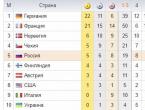
Differential Diagnosis The most common walking disorders are schematically presented in the figure.
There are several types of such violations.
Walking in small steps with freezing» at the beginning of movement and when turning, it is characteristic of parkinsonism syndrome and lesions of the frontal cortex (with hydrocephalus, tumors of the frontal regions, frontal dementia, vascular encephalopathy). In parkinsonism syndrome, there is also a bent position of the body and bent arms, shuffling when walking. Lesions to the frontal lobe are characterized by "sticking" of the feet to the floor ("magnetic" gait) and/or apraxia of walking (as well as apraxia of the feet and legs in general when sitting).
In the latter case, join as well as cognitive impairment. urination disorder and the so-called frontal motor disorders (revival of grasping, perioral reflexes, facilatory paratonia, etc.), which in Parkinson's disease appear only in the later stages of the disease.
spastic(with legs dragging, sometimes with clonuses) or spastic-atactic gait: damage to both legs (paraspastic) - primarily with pathological processes in the spinal cord (for example, with multiple sclerosis, Arnold-Chiari malformation); damage to half of the body (hemispastic) - primarily with supraspinal pathology (for example, a condition after a stroke).
Atactic. with lesions of the cerebellum (with legs wide apart, with lateropulsions, ipsilateral to the focus, in most cases also with ataxia of the trunk in a sitting position, and sometimes only with discrete ataxia in the extremities), with vestibulopathy (with lateropulsions, contralateral to the focus), with polyneuropathies (with violations of the vibration sense and the sense of position in space and a positive Romberg test).
Occasionally observed atactic gait in the absence of paraspastic disorder and with lesions of the spinal cord (epidural metastases) (see above). Ataxia of the legs and atactic gait can also be observed when the frontal lobe is affected (sometimes it is a wide-legged gait, the so-called Brun's ataxia).

Paretic. with polyradiculopathy, polyneuropathy (sometimes steppage is observed) and myopathies (may be accompanied by Trendelenburg or Duchenne lameness). Depending on the severity of the lesion, paresis may be accompanied by ataxia of the affected limb and ataxia of walking.
Difficult classifiable walking disorder(atactic, pretentiously grotesque, "acrobatic", with sudden incomprehensible freezing in an unusual position, changeable, with bouncing, etc.): with choreic syndromes (primarily with Huntington's chorea; walking disorders are often regarded as psychogenic at first), dystonia (with Wilson's disease, with dopamine-sensitive dystonia (Segawa's disease) in children). Manganese poisoning is characterized by a gait on the tips of the fingers with an overbent torso (“cock walk”).
Only after exclusion these movement disorders psychogenic gait disorder may be suspected. The latter is characterized by improvement in distraction, dissociation between walking backwards and forwards (the latter is paradoxically worse).
non-specific. in the case of a predominance of uncertainty when standing over gait disturbance, orthostatic tremor can be assumed.
Most of these walking disorders discussed in more detail elsewhere in the book. Special mention should be made of multifactorial gait disorder common in older age:
For senile walking disorders characterized by small, uncertain steps, a bent posture and meager hand movements. It resembles the gait of a patient with parkinsonism, but there are no other manifestations of this disease (tremor, rigidity, hypokinesia). In older people, walking impairment is complex, it is based on a number of reasons, including non-neurological ones, which generally leads to unsteady gait and falls:
- the use of certain drugs (sdative, hypnotics, antiepileptic drugs, antidepressants, etc.);
- orthostatic hypotension (including due to side effect medicines);
- visual impairment;
- vestibulopathy;
- orthopedic and rheumatic diseases (coxarthrosis, gonarthrosis, foot deformities, etc.);
- mental factors, in particular, the fear of taking the first step.
Some of them factors can be corrected with treatment.
— Return to the table of contents of the section « Neurology. "
Cardiologist
Higher education:
Cardiologist
Kuban State medical University(KubGMU, KubGMA, KubGMI)
Level of education - Specialist
Additional education:
"Cardiology", "Course on magnetic resonance imaging of the cardiovascular system"
Research Institute of Cardiology. A.L. Myasnikov
"Course on functional diagnostics"
NTSSSH them. A. N. Bakuleva
"Clinical Pharmacology Course"
Russian Medical Academy of Postgraduate Education
"Emergency Cardiology"
Cantonal Hospital of Geneva, Geneva (Switzerland)
"Course in Therapy"
Russian State Medical Institute of Roszdrav
Movement disorders are the most common complications of stroke. They are observed in more than 80% of patients. Of these, only 20% are fully restored. The effectiveness of rehabilitation depends on the timeliness of medical care at the onset of a stroke, as well as on how early rehabilitation treatment began. The most effective it will be the first six months after a stroke and the completion of intensive care.
Why is walking impaired?
During an ischemic stroke, areas of the brain responsible for motor functions remain without nutrition. These are sections of the pyramidal system, with the help of which a person makes conscious (voluntary) movements. Depending on the site of ischemia and the degree of damage, complete paralysis or paresis of certain muscles develops.
Special brain cells generate impulses to start movement, which are conducted to the muscles using a complex system of neurons. When some of them are turned off from the process, the muscle does not receive commands "from above" and remains motionless. At the same time, all possible motor programs are stored in the "card file" of the lower motor system.
The task of motor rehabilitation is to restore the lost connections between the brain and muscles, help the body "remember" the necessary motor programs and restore the ability of the brain to control them.

With it to start recovery?
The first thing done after a stroke to prevent loss of motion in the joints and tendons is treatment with position. To do this, the leg is fixed in a straightened position with a slight turn inward and the foot resting on the headboard. Fixation is carried out within 1.5 - 2 hours.
Passive exercise
Recovery of walking after a stroke begins with the training of individual muscles and joints. A stroke usually affects one hemisphere of the brain. In this case, they speak of hemiparesis or hemiparalysis - a unilateral impairment of motor functions. Restoration of movements in a sore leg begins with passive exercises.
They are performed by an exercise therapy specialist, gradually including the patient himself in the process, that is, gradually transferring passive movements into active (controlled) ones. The set of exercises includes:
- flexion, extension and rotation of the feet;
- flexion and extension of the knee;
- flexion, extension and abduction at the hip joint.
If the patient understands well what is required of him, his consciousness must be involved in the process. He must learn to send an impulse to an immobile muscle. To do this, the exercise is done independently with a healthy leg, and then the movement is mentally transferred to the sore leg. The use of muscle memory is perhaps the most important component of the entire rehabilitation process.

Translation of movements into the active phase
The mental message should not fit only in the time allotted for gymnastics. A person striving for a speedy recovery and gaining lost skills should practice throughout the day with short breaks for food, toilet, procedures and sleep.
As the muscle regains strength through passive exercise, the patient must be encouraged to move independently. The assistant sets the amplitude of the movement, and the patient himself must perform it. The movement should be slow and done in parts.
Walking after a stroke is restored with the following exercises:
- Flexion and extension of the legs at the knees. At the same time, the feet slide on the bed. It is performed alternately with the diseased and healthy leg.
- Switching legs. Legs bent at the knees, feet resting on the bed. A healthy leg should be thrown over a sick one, and then vice versa.
- A similar exercise, only one leg should be put on the knee, moving it to the side, then repeat the exercise with the second leg.
- Bicycle exercise.
- Stop turns. Legs are bent at the knees, feet are on the bed. Turning the feet out and in.
- Lying with straightened legs, alternately run the heel of one leg along the front of the lower leg of the other.
- Raising and abducting the legs of the side.
- Raise the pelvis, lying with bent knees.
- Lying on your stomach, bend and unbend your knees.
- Lying on your side, raise your leg.
- Side Turns (restores the skill of turning over in bed). Lying on your back, lower your bent knees to the side, then complete the turn with your torso.

All exercises begin with a healthy leg. You should not immediately ask many approaches to perform one exercise. The number of repetitions depends on the condition of the patient and is increased with great care.
Transfer to a sitting position
A great achievement is the ability of the patient to sit on the bed independently, and most importantly, to maintain this position. Move it to a vertical position gradually and carefully to avoid dizziness and pressure buildup.
After mastering the skill of turning over the patient lying on his side, you need to slowly seat him - the legs are lowered from the bed, the healthy hand is repelled from it. His feet should be resting on the floor and slightly apart, the body is slightly tilted forward to maintain balance.
getting up
The next step is getting up. For training, several exercises are used:
- lifting on the bed - first with the help of an instructor, then - a gradual transition to independent lifting;
- moving along the edge of the bed from back to back - moving the legs on the floor and moving the patient away from the fulcrum of the legs so that he pulls them up on his own.
After lengthy training, the muscles and consciousness of the patient are already ready to get up and hold the body in an upright position. It is important to ensure his safety, as a fall can be frightening and make the patient refuse the next attempt for a long time. Getting up should take place with additional support and the help of an outsider. Trainings are accompanied by explanations of how certain movements are performed correctly. The patient will mentally remember them, stimulating the brain to send impulses.

Before the patient takes the first steps, standing skills are reinforced with exercises:
- Trampling is the transfer of the center of gravity from one foot to another, as if a person is shifting from foot to foot. First, the exercise is performed without lifting the feet off the floor, then they need to be slightly raised.
- Rolling from toe to heel.
- Stepping over an obstacle - at first it can be a pencil, then the height is increased. When performing, the knee should rise high. Steps are taken forward and backward.
- Leading the legs back (the leg is placed on the toe).
Walking recovery
The assistant helps his ward, supporting him from the healthy side. He, as it were, makes a jerky movement, prompting the patient to rearrange the sore leg, and then lean on it.
If it is difficult for one person to cope with learning to walk a post-stroke patient, the help of another person will be needed to rearrange the patient's diseased leg. This happens when the patient is not quite adequate or has a lot of weight.
It is good to alternate daily walking training with exercises on the carpet:
- turning from side to side;
- rolling from one edge of the carpet to the other;
- head lifts;
- getting up on all fours and moving in this position;
- plastunsky crawling.
For these exercises, the instructor will also need an assistant.
Massage to restore walking
It is difficult to overestimate the role of massage in restoring all body functions after a stroke. This is especially true for motor injuries. An experienced massage therapist does not use certain strictly limited techniques. He always proceeds from their condition of the patient and finds by experience an individual way of massage.
Not only a paralyzed leg or arm is subjected to massage. The entire damaged side of the body is massaged, starting from the scalp, ending with the toes. The procedure effectively restores blood circulation in numb skin and muscles, as well as the sensitivity of nerve endings. Massage courses begin 3-4 days after the stroke and should continue for the next year or even two years. The usual manual massage will be successfully complemented by hydromassage and underwater shower.
How to ensure safety when restoring walking?
Falling after a stroke can lead to injury. Most often, such patients break the hip of the diseased leg. The reasons may lie not only in the lack of stability of the patient, but also in the imperfection of the environment. It can be slippery floors, too long pile carpets, poorly installed handrails in the bathroom and toilet, and simply insufficient supervision of a sick person.
At the initial stage, when the patient does not feel very confident, special devices will help - a three- or four-point crutch, a walker. To avoid back bending of the knee joint, an orthosis is used to fix the knee in the desired position.
Usually, aids are prescribed by the attending physician. He will also determine the deadlines for waiving them. Some fixtures are worth using all the time, for example, handrails in the bathroom.
How long will recovery take?
The possibility of rehabilitation of walking after a stroke and the recovery time depend on many factors - the initial severity of a motor defect (for example, paralysis in the acute stage of a stroke), increased muscle spasm or, on the contrary, their hypotrophy, concomitant musculo-articular disorders.
Significantly inhibits the recovery of cognitive impairment, decreased mental activity, loss of interest in life and depressive states. And vice versa, a well-timed and regularly carried out complex of rehabilitation measures significantly accelerates the restoration of lost functions. Specific terms of the recovery period are individual.
Why is walking important for overall recovery after a stroke?
Having regained the ability to walk independently, the person is ready for further social rehabilitation. Next, a gradual restoration of the ability of self-service, and then household skills, is carried out.
Restoration of movement gives impetus to the restoration of other body functions. The successes that the patient makes and which must necessarily be emphasized by the people surrounding the "stroke", contribute to the restoration of the psycho-emotional state. And this, in turn, gives an incentive to strong-willed efforts, without which full-fledged rehabilitation is simply impossible.
Ataxia after a stroke - symptoms, diagnostic tests, treatment
Ataxia is one of the types of movement disorders that occurs in patients after a stroke. This is a collective concept that includes several types of impaired coordination of movements. In clinical practice, cerebellar ataxia is most common, the cause of which is a violation of blood circulation in the cerebellum. According to statistics, cerebellar stroke is not so common - in about 10% of cases.
However, more than half of the episodes of this type of stroke end in death, and a very high percentage of disability is recorded among the survivors.
Ataxia is a violation of coordination of movements and motor skills.
Classification of ataxias
Normally, coordination of movements is regulated by the following parts of the brain:
- medulla oblongata and midbrain;
- cerebellum;
- vestibular apparatus;
- frontotemporal cortex of the cerebral hemispheres.
In the posterior part of the brainstem are the bundles of Gaulle and Burdach. They are responsible for deep muscle sensitivity. The main task of the cerebellum is to complement and coordinate the work of the motor centers. Thanks to him, the movements become smooth, clear and proportionate. The cerebellar vermis maintains normal muscle tone and balance. Thanks to the coordinated activity of the vestibular nuclei, balance is maintained during movements. The frontal cortex is responsible for voluntary movements.
It is difficult to say which of these departments is the most important in the coordination of movements. All of them are connected by numerous synaptic connections, which ensures normal motor activity. Depending on where the stroke occurred, clinicians distinguish between the following types of motor coordination disorders, or ataxias:
Sensitive ataxia
This type of ataxia develops after a stroke in the posterior columns of the spinal cord, the thalamus. It can appear in both limbs, one arm or one leg. This type of movement disorder is characterized by loss of proprioceptive sensitivity. The patient cannot assess the position of his own body parts. There is a so-called stamping gait - the patient bends his legs excessively and steps very hard on the floor. Often complains of the sensation of walking on soft carpet. The victim constantly looks at his feet, thus trying to alleviate the pathological symptoms. When the eyes are closed, the manifestations of ataxia intensify.
Cerebellar ataxia
Develops after a cerebellar stroke. There is unsteadiness when walking. The patient deviates towards the lesion, in severe cases falls. If the cerebellar vermis is affected, a fall is possible in any direction and backwards. Walking is wobbly, with legs wide apart. Walking with a side step is impossible or sharply impaired. Hand movements are disproportionate, slowed down. The arm and leg on the side of the lesion are most affected. Speech slows down, becomes drawn out, chanted. In contrast to aphasia, where the basis of speech disorders is the death of neurons in the cortical centers, in patients after a cerebellar stroke, coordination of movements is disturbed. The handwriting changes - the letters become sweeping, large.

Distinctive features of the gait of a patient with ataxia
vestibular ataxia
Vestibular ataxia is manifested when moving, sitting or standing. Symptoms are aggravated by turning the head, trunk, eyes. The person refuses to perform these movements, replaces them with others or performs at a slow pace. Thanks to visual control, it is possible to significantly compensate for impaired coordination. With a unilateral lesion of the vestibular nuclei, shakiness and deviations of the body occur in the direction of the lesion. Movement disorders are especially noticeable when walking with closed eyes. Vestibular ataxia is accompanied by severe autonomic disorders - nausea, dizziness, nystagmus.
Cortical ataxia
A specific disorder of coordination of movements that develops in patients after a stroke in the frontal lobe of the cerebral hemispheres. Mostly in such situations, the legs suffer. The hands are not involved. The patient's gait is uncertain, shaky, along one line. The body leans back. The patient cannot stand and walk, despite the fact that he has no signs of paresis or paralysis.

Clinical manifestations of cortical ataxia
Diagnostic tests
Diagnosis of impaired coordination of movements in patients after a stroke is based on the following points:
- patient complaints;
- inspection data;
- diagnostic test results;
- data from the results of additional research methods.
Coordinating tests allow you to determine the type of ataxia, to establish the location of the stroke.
The first is static ataxia. The patient is placed in the Romberg position - legs together, arms forward, eyes closed. The stability of the patient is assessed. After the usual Romberg test, a complicated one is carried out - they are asked to stretch their hands in front of them at shoulder level, spread their fingers to the sides, put their legs so that the toe of one touches the heel of the second limb.

Study of the function of the cerebellum
Then the gait is evaluated. The patient is asked to walk in a normal gait in a straight line, heel to toe and flank gait.
After that, the diagnosis of dynamic ataxia is carried out. The patient is asked to extend his arms in front of him and reach the tip of the nose or the malleus with the index finger. The test is carried out with open and closed eyes.
The symmetry and synchronism of movements can be assessed using an asynergy test - the patient is asked to stretch his arms in front of him and make movements similar to screwing in light bulbs. Another diagnostic test is for dysmetria. The patient needs to raise both hands to shoulder level and stretch them in front of him. After that, you need to raise one hand vertically up and lower it to the level of the second. The test is repeated on the opposite side.
Heel-knee test - in the supine position, the patient should touch the heel of one leg to the opposite knee.
Asinegria Babinsky - the patient is asked to sit down with his arms crossed over his chest. If the cause of impaired coordination of movements is in the cerebellum, it is not the body that rises, but the legs.
Treatment
In patients after a stroke, in the first hours after the disease, the resumption of blood circulation in the focus of necrosis comes to the fore. Then nootropic and vascular agents are prescribed. Their main task is to reduce the size of the focus, to help the surviving neurons integrate into the overall activity of the central nervous system.
As soon as it becomes possible, the patient begins motor gymnastics.
To improve coordination, it is necessary to perform complex purposeful actions - to lift small objects from the floor, to open locks, to “catch up” with moving objects with your hands, to press buttons located at some distance from the patient. If it is necessary to coordinate the movements of two joints, then one of them is fixed and movements are carried out without it.
With vestibular ataxia, exercises are carried out with an increase and decrease in the area of \u200b\u200bsupport, with the elimination of visual control - in the dark, blindfolded, with headphones. It is recommended to walk on uneven terrain, backwards, on a stencil. It is very useful to combine such exercises with gymnastics for the eyes.
An important role is played by massage, passive gymnastics, physiotherapy procedures.
How to restore coordination of movements
Article from our subscriber
One of the main disorders that a stroke caused is a severe loss of coordination of movements. I couldn't do the simplest test. Stretch your arms forward, close your eyes and touch the tip of your nose with your left and right hands. I missed. Right hand not much. Instead of the tip of the nose, it fell into the bridge of the nose. With his left hand he missed hard, hit the forehead area, or even missed his head altogether.
Recovery after a stroke is not possible without the restoration of coordination. To make any movement requires not only muscle strength. Their work needs to be coordinated.
In the beginning, I couldn't put a teaspoon into a cup. Didn't hit.
Stronger coordination is disturbed on the left side. But we don't more exercise to the left side. Everything balances out gradually in the course of training.
Beginner level exercises
To restore coordination, we do special gymnastics. We picked up exercises for working out exactly those movements with coordination of which there is a problem. As we recover, we complicate the gymnastics. Therefore, several gymnastics came out. Here is the gymnastics we started with. Some of the exercises we started doing in bed.
1. Touching the nose
- I do it while sitting in bed.
- I extend both hands in front of me.
- I close my eyes.
- alternately touch the tip of the nose with the fingers of the right and left hands.
- 10 reps.
2. Chess with the right hand
- I do it while sitting in bed.
- I place the pieces on the chessboard with my right hand.
- 5 repetitions.
3. Chess with the left hand
- I do it while sitting in bed.
- I place the pieces on the chessboard with my left hand.
- 10 reps.
4. Square with the right hand
- I do it while sitting in bed.
- I draw a square with my right hand. In front of you, at arm's length. At face level.
- 10 reps.
5. Square left hand
- I do it while sitting in bed.
- I draw a square with my left hand. In front of you, at arm's length. At face level.
- 10 reps.
6. Circle with the right hand
- I do it while sitting in bed.
- I draw a circle with my right hand. In front of you, at arm's length. At face level.
- 10 reps.
7. Left hand circle
- I do it while sitting in bed.
- I draw a circle with my left hand. In front of you, at arm's length. At face level.
- 10 reps.
8. Two squares
- I do it while sitting in bed.
- with both hands simultaneously and synchronously “draw” two squares. In front of you, at arm's length. At face level.
- 10 reps.
9. Two circles
- I do it while sitting in bed.
- with both hands simultaneously and synchronously “draw” two circles.
- 10 reps.
- In front of you, at arm's length. At face level.
10. Left leg circle
- I do it sitting on the edge of the bed.
- with the toe of the left foot I “draw” a square on the floor.
- 10 reps.
11. Right leg circle
- I do it sitting on the edge of the bed.
- with the toe of the right foot I “draw” a circle on the floor.
- 10 reps.
12. Square feet
- I do it sitting on the edge of the bed.
- with two legs synchronously with toes I “draw” a square on the floor.
- 10 reps.
13. Circle with legs
- I do it sitting on the edge of the bed.
- with two legs synchronously with toes I “draw” a circle on the floor.
- 10 reps.
Improvement Rules
When drawing figures, I try to make the figures even and neat. Exercises are performed slowly, smoothly and calmly.
The exercises are very simple. We started doing them three weeks after the stroke. The result from them is noticeable and obvious. We did gymnastics five times a week. A month later, the coordination of movements and arms and legs greatly improved.. More difficult exercises began to turn out.
Any movement you make is a micro workout for coordination. It is important to think before doing something. Even to just reach out to the cup and take it, you need to think about what and how you are doing. Every movement is registered and remembered in the brain, especially repeated many times. This is the skill.
We realized that if the movements are done slowly and smoothly, then they are easier to coordinate and do correctly. As a result, the correct movement is recorded in the brain, and not an error. Plus, with smooth and slow movements, I did less devastation and did not cling to the objects around me. So the most effective way recovery of coordination, it is control over every movement and smoothness.
Advanced exercises
But this does not cancel special exercises. Correct gymnastics consists of movements more complex than in life. Therefore, having learned to do the complex, then it is easy to do the simple. We see the point sports training in recovery after a stroke. Skiing, cycling or long walks make millions of movements.
There is a training of strength and endurance. Coordination of movements is worked out and fixed. In ordinary life, there are no such loads and complex movements as in sports. Therefore, after training, simple and ordinary skills are actively restored.
Moving from "lying", bed rest to "walking" and slightly restoring the initial coordination skills, we moved on to more complex gymnastics:
14. Figures with the right foot
- hands on the belt.
- I shift my weight onto my left leg. The right leg is fully unloaded
- with the toe (thumb) of the right foot, straight in front of me, I draw figures on the floor in order (circle, square, triangle).
- I draw figures of medium size, so that it would be convenient and not have to stretch.
- 3 repetitions x 3 figures.
15. Figures with the left foot
- I do it standing. If it is needed. I do it with support.
- hands on the belt.
- I shift my weight to my right foot. The left leg is completely unloaded.
- with the toe (thumb) of the left foot, straight in front of me, I draw figures on the floor in order (circle, square, triangle).
- 3 repetitions x 3 figures.
16. Numbers with the right foot
- I do it standing. If it is needed. I do it with support.
- hands on the belt.
- I shift my weight onto my left leg. The right leg is completely unloaded.
- with the toe (thumb) of the right foot, straight in front of me, I draw numbers on the floor, in order from 1 to 10.
- I draw figures of medium size, so that it would be convenient and do not have to stretch.
- 2 repetitions x 10 digits.
17. Numbers with the left foot
- I do it standing. If it is needed. I do it with support.
- hands on the belt.
- I shift my weight to my right foot. Left leg fully unloaded
- with the toe (thumb) of the left foot, straight in front of me, I draw numbers on the floor, in order from 1 to 10.
- 2 repetitions x 10 digits.
We perform these exercises smoothly. While “drawing” figures or numbers on the floor, I make movements smoothly and slowly. The main quality of the "drawing". With such exercises we train coordination, this is the main thing. Therefore, at the beginning I did them with support.
To not worry about balance. Standing on my left foot makes it harder for me to keep my balance. Standing on my right foot, I keep my balance confidently, but at the same time, “drawing” with my left foot is not very good. Just when performing such exercises, jambs with coordination come out. We are catching them.
![]()
Leave a reply

Is there a risk of stroke?
1. Increased (more than 140) blood pressure:
- often
- Sometimes
- rarely
2. Atherosclerosis of vessels
3. Smoking and alcohol:
- often
- Sometimes
- rarely
4. Heart disease:
- birth defect
- valvular disorders
- heart attack
5. Passage of medical examination and diagnostic MRI:
- Every year
- once in a lifetime
- never
Total: 0%
Stroke is a rather dangerous disease, which affects people far from only old age, but also middle and even very young people.
A stroke is an emergency situation that requires immediate help. It often ends in disability, in many cases even death. In addition to blockage of a blood vessel in the ischemic type, a cerebral hemorrhage against the background of high blood pressure, in other words, a hemorrhagic stroke, can also cause an attack.
A number of factors increase the chance of having a stroke. For example, genes or age are not always to blame, although after 60 years the threat increases significantly. However, everyone can do something to prevent it.
1. Avoid hypertension
High blood pressure is a major risk factor for stroke. Insidious hypertension does not show symptoms at the initial stage. Therefore, patients notice it late. It is important to have your blood pressure checked regularly and take medications for elevated levels.
2. Quit smoking
Nicotine constricts blood vessels and raises blood pressure. A smoker is twice as likely to have a stroke than a non-smoker. However, there is good news: those who quit smoking significantly reduce this risk.
3. With excess body weight: lose weight
Obesity is an important factor in the development of cerebral infarction. obese people should think about a weight loss program: eat less and better, add physical activity. Older people should talk to their doctor about the extent to which they benefit from weight loss.
4. Keep cholesterol levels normal
Elevated levels of “bad” LDL cholesterol lead to deposits in the vessels of plaques and embolism. What should be the values? Everyone should find out individually with a doctor. Since the limits depend, for example, on the presence of concomitant diseases. In addition, high values of "good" HDL cholesterol are considered positive. A healthy lifestyle, especially a balanced diet and plenty of exercise may positively affect cholesterol levels.
5. Eat healthy food
Useful for blood vessels is a diet that is commonly known as "Mediterranean". That is: lots of fruits and vegetables, nuts, olive oil instead of cooking oil, less sausage and meat, and lots of fish. Good news for foodies: you can afford to deviate from the rules for one day. It is important to eat right in general.
6. Moderate alcohol consumption
Excessive alcohol consumption increases the death of stroke-affected brain cells, which is unacceptable. Complete abstinence is not required. A glass of red wine a day is even helpful.
7. Move actively
Movement is sometimes the best thing you can do for your health in order to lose weight, normalize blood pressure and maintain the elasticity of blood vessels. Ideal for this endurance exercise, such as swimming or brisk walking. The duration and intensity depend on the personal physical training. Important Note: Untrained people over 35 years of age should be initially examined by a doctor before starting to exercise.
8. Listen to the rhythm of the heart
A number of heart conditions contribute to the likelihood of a stroke. These include atrial fibrillation, birth defects, and other rhythm disturbances. Possible early signs of heart problems should not be ignored under any circumstances.
9. Control your blood sugar
People with diabetes are twice as likely to have a cerebral infarction than the rest of the population. The reason is that elevated glucose levels can damage blood vessels and promote plaque buildup. In addition, diabetic patients often have other risk factors for stroke, such as hypertension or too high blood lipids. Therefore, diabetic patients should take care of the regulation of sugar levels.
10. Avoid stress
Sometimes stress has nothing wrong, it can even motivate. However, prolonged stress can increase blood pressure and susceptibility to disease. It can indirectly cause a stroke. There is no panacea for chronic stress. Think about what is best for your psyche: sports, an interesting hobby, or perhaps relaxation exercises.
Consequences of a stroke - impaired speech functions
Stroke is a serious disease, dangerous with many severe consequences, which, in addition, can have death. Speech impairment during a stroke is a consequence that overtakes 2 out of 3 victims as a result of an apoplexy.

Aphasia is an impairment in the ability to use or understand words. It usually occurs if the stroke affects the right side of the body.
Aphasia can cause difficulties:
- in the understanding of words;
- in search of suitable words expressing thought;
- in understanding oral speech;
- in reading or writing words or sentences.
Generally, aphasia can be divided into four broad categories:

Symptoms of the disease
A stroke is a blockage or rupture of blood vessels. The ability to recognize the signs of a stroke in time makes it possible to act quickly and avoid many problems, since this disease puts a person’s life at risk. It is important not to waste a single minute, as the risk of brain damage increases. After a stroke, about two million brain cells die every minute if treatment is not started on time. The elderly are at greater risk, although this devastating disease can occur at any age.
Since a stroke is a disease of the brain, often the person himself cannot understand what is happening to him. Need outside help.
Here are some important signals and signs of a stroke:

Cause of stroke
The most common is an ischemic stroke, which results from a blockage or narrowing of a blood vessel. A hemorrhagic stroke occurs due to the rupture of a blood vessel in the brain. This species is less common but has more serious consequences.
Factors that provoke the development of a stroke:

In addition, the cause of a stroke can be hypertension, atherosclerosis, or cerebral aneurysm. The disease can be prevented by destroying the factors predisposing to its development. Many of them can be changed by the person himself, getting rid of bad habits, leading healthy lifestyle life and eating right.
Why do people lose the ability to speak when they have a stroke?
The brain controls various bodily functions. If a stroke occurs and blood flow cannot reach an area that controls a particular bodily function, that organ will not function properly. Speech impairment after a stroke occurs due to damage to the speech areas of the brain: Wernicke's and Broca's areas.
 When a stroke affects the part of the brain that controls the muscles used to produce speech, speech can become slurred, causing dysarthria. And if there is damage to the part of the brain that controls language, the affected person may lose the ability to speak and understand speech (aphasia).
When a stroke affects the part of the brain that controls the muscles used to produce speech, speech can become slurred, causing dysarthria. And if there is damage to the part of the brain that controls language, the affected person may lose the ability to speak and understand speech (aphasia).
The time to restore speech ability after a stroke depends on the degree and site of brain damage, the age of the patient, and how quickly first aid is provided. The process is lengthy, since it is necessary to restructure the intact areas of the brain to perform conversational functions. It takes longer than the recovery of motor functions. The effectiveness of rehabilitation measures is observed during the first 6 months after a stroke. During this period, you can achieve high results.
 A stroke that affects one side of the brain will lead to neurological complications on the opposite side of the body. Paralysis of the right side of the body indicates that left-sided damage to the cerebral cortex has occurred. Since the areas of the brain responsible for speech functions are located in the left hemisphere, patients with this disorder have a less favorable prognosis. Patients with left-sided paralysis have a more favorable prognosis.
A stroke that affects one side of the brain will lead to neurological complications on the opposite side of the body. Paralysis of the right side of the body indicates that left-sided damage to the cerebral cortex has occurred. Since the areas of the brain responsible for speech functions are located in the left hemisphere, patients with this disorder have a less favorable prognosis. Patients with left-sided paralysis have a more favorable prognosis.
In the first hours and days after a stroke, a person may completely lose speech. Therapy should be started as early as possible after the patient regains consciousness.
Therapy for speech disorders
Full recovery after speech impairment is possible. Speech therapy is the most common treatment for the disease. There are various specific speech therapy exercises and techniques.
Other widely used therapies for stroke survivors that have been shown to be effective include:

It is important to continue treatment at home. It includes:
- Playing word games.
- Writing greeting cards, recipes, shopping list.
- Reading and singing aloud.
In the process of communicating with a person who has had a stroke, it is necessary to be patient, provide support and understanding.
Some tips for communicating with a person after a stroke:

Folk methods for restoring speech functions
After treatment in the conditions of medical institutions, continued therapy at home is indicated. In this case, it is possible to use traditional medicine, but only after consulting with your doctor. Among the most common traditional medicine is considered to be a product of alternative medicine of natural origin mummy. This drug, which is available in the form of a balm or tablets, promotes the regeneration and formation of cells that form tissues and organs, increases the elasticity of blood vessels. There are several recipes using mummy:

Also effective in speech disorders is the use of baths with essential oils. Coniferous baths contribute to relaxation, normalization of the psycho-emotional background.
Massage and exercises to restore speech
To restore speech functions, special exercises are effectively used, the essence of which is to train the speech muscles.
The following set of exercises is performed:

The cause of speech impairment after a stroke may also be paralysis of facial muscles. In this case, physiotherapeutic procedures, massage and physiotherapy exercises will be effective. Acupuncture, electromyostimulation, etc. are widely used.
The use of physical therapy is to perform a set of physical exercises, breathing exercises, passive exercises for different groups muscles.
Regular speech therapy massage helps to stimulate all speech zones, which also has a beneficial effect on the process of recovery and normalization of speech after a stroke.
Stroke is a very common disease that has a high mortality rate in the world. But knowing the causes and symptoms, you can prevent it or reduce the level of negative consequences for a person.
Consequences of a stroke
Hello, dear readers and guests of the site dedicated to neurorehabilitation. Let's talk today and take a closer look consequences of a stroke- ischemic and hemorrhagic, as well as everything connected with this.
 Consequences of a stroke.
Consequences of a stroke.
Violations of any functions after a stroke are directly dependent on its severity, and severity, in turn, on the size of the focus and its location in the brain.
Of course, it would be fair to note that the size of the focus and its localization are far from all factors that determine the persistence of the depth of neurological disorders caused by a stroke, the consequences of which (the nature and severity) can vary greatly, depending on the specific case. What does it depend on?
The degree of dysfunction after a stroke is not always persistent. With a small stroke, the consequences may be minimal or even absent, but this does not happen so often. We will discuss cases when these consequences are present and they are persistent. We will analyze in more detail what exactly the consequences of a stroke are and how they are expressed. Below are the most significant violations of body functions that occur after a stroke.
Right-sided and left-sided hemiparesis after stroke.
One of the most common persistent consequences of a stroke is a decrease in strength in half of the body - hemiparesis. As a rule, after a stroke, there is a decrease in muscle strength in one of the sides of the body, which is opposite to the damaged hemisphere of the brain: if hemiparesis of the left side of the body is a persistent consequence, the stroke occurs in the right hemisphere. By the same principle, hemiparesis of the right side of the body, in which a stroke is observed in the left hemisphere. That is, the focus of infarction in the brain is located in the opposite hemisphere of the affected half of the body.
It also happens that a stroke leads to a complete lack of muscle strength in half of the body, which is called hemiplegia. With hemiparesis, a person experiences difficulty in moving, with hemiplegia, the difficulties are even more significant. Simply put, hemiplegia is paralysis in half of the body (complete lack of movement).
Habitual movements in the body are disturbed, many people have to learn to perform normal daily activities again in order to be able to take care of themselves, be able to eat, change clothes and walk. In general, to do everything that before the illness was considered extremely simple and ordinary to perform. It is the decrease in muscle strength in half of the body that is the main reason for the disability of a person after suffering a violation of cerebral circulation. It is because of this that patients lose the ability to move independently - or lose this ability completely or it is significantly impaired.
As you have already described, gait after a stroke can often be disturbed, while a person begins to move with great difficulty. In some cases, assistive devices may be needed - special walkers, a support cane or a crutch. A characteristic Wernicke-Mann posture develops when walking. Individual parts of the body may be affected without involving the entire half of the body. Depending on the affected half of the body, there are left-sided and right-sided hemiparesis.
Central prosoparesis.
The next, one of the most common consequences, is the so-called central prosoparesis, in which the mimic muscles suffer, resulting in facial asymmetry, as in Figure 1. At the same time, a decrease in strength is observed not in the entire half of the face, but only in its lower part, capturing the mouth, cheek, lips.
The eyelids and eyes with this paralysis of the mimic muscles remain unaffected, despite this, the distortion is quite noticeable and causes discomfort not only during meals or liquids. Central prosoparesis regresses with recovery from stroke.
With central prosoparesis, food intake and fluid intake are difficult. A person experiences obvious discomfort when performing some actions with facial muscles. Habitual emotions are more difficult to express, due to a decrease in strength in facial muscles sound formation is disturbed and speech begins to suffer.
The defect itself brings a tangible inconvenience purely from the cosmetic side. Distortion of the face causes great emotional discomfort, especially when communicating with other people. This can cause isolation and renunciation of communication with others and cause deep depression.
Speech impairment after stroke.
Speech disorders after a stroke are also quite common, at the same time it is one of the very first signs of an onset (upcoming) cerebrovascular accident. Speech impairment is the result of damage to the speech centers of the brain, which is a partial or complete loss of the ability to speak and perceive someone else's speech, called aphasia.
According to statistics, such violations are observed in a quarter of all people who have experienced a stroke, their consequences can be quite persistent. Sometimes it is difficult for a person to speak, due to a violation of the possession of the speech apparatus, and the speech of such people is fuzzy, as if “porridge in the mouth”, and such a violation is called dysarthria . dysarthria more common in stem stroke or localization of this focus in the cerebral cortex. The next speech disorder is aphasia.
Aphasia is the complete absence of speech. Aphasia can be of several types, to name some of them - with the defeat of the speech center responsible for the pronunciation of speech, motor aphasia develops. When the focus of the stroke is located in the center of speech, which is responsible for its perception, the so-called sensory aphasia develops. With sensory aphasia, a person does not understand what is being said to him and does not understand what he needs to answer. If both centers are affected, mixed or sensory-motor aphasia. The "pure" form of aphasia is extremely rare, and with a stroke, it is the mixed form that most often occurs.
There are other types of speech disorders after a stroke, which we will discuss in detail in the following articles on speech disorders. And now let's move on ... In addition to the violations listed above, there are the following consequences of a stroke.
Disturbances in coordination of movements after a stroke.
Impairment of blood circulation in the parts of the central nervous system responsible for the coordination of movements and as a result of a stroke can lead to coordination of movements, which is called ataxia. Disturbances in coordination of movements often occur with stem stroke and this is due to the fact that in the stem part of the brain there are centers for coordinating movements in our body.
There are different degrees of expression. In the most favorable case, these vestibular disorders disappear within the first day after the acute cerebrovascular accident. In other, more severe cases, unsteadiness when walking and dizziness persist for a longer period and may last for months.
visual impairment after stroke.
There may be visual impairments of the most diverse nature. Visual impairment depends on the location of the stroke and the size of the focus. Most often, visual impairment manifests itself in the form of loss of visual fields (hemianopia). In this case, as you may have guessed, half or a quarter of the visual picture falls out. If a quarter of the picture falls out, it is called a quadrant hemianopia.
Other consequences of a stroke.
- Hearing impairments (hypoacusia), smell impairments (hypo-, anosmia), loss of movement skills with the strength stored in them (apraxia) and other disorders that can and should be treated, rehabilitation in this case is very important and should be carried out in a timely manner.
- Loss of sensation after a stroke. Violation of sensitivity after a stroke can be of a different nature, but most often it is a loss of the ability to feel pain, recognize heat, cold, and a part of the body as such. It is also possible the appearance of pain syndrome, which is of the most diverse nature and localization. Most often, there is a decrease in sensitivity in any part of the body, this phenomenon is called hypesthesia.
Depression after a stroke.
Depression- another consequence of a stroke that can cross out any efforts of a doctor and loved ones to restore lost functions. According to some reports, up to 80% of stroke survivors suffer from depression in varying degrees of severity. This is a rather serious consequence that can and should be treated.
In addition to the mood for recovery, an additional no less important “bonus” of eliminating depression will be an analgesic effect. It has long been proven that depression can increase pain in a person, and pain in a stroke is not uncommon. Prescribing antidepressants can help with this problem.
It is extremely important to prescribe the “correct” antidepressant, since some of them can cause an “inhibitory effect”, which in some cases can also reduce a person’s desire to follow the doctor’s recommendations and activate for better rehabilitation.
A stroke, the consequences of which remained after a course of treatment in a hospital, is a frequent phenomenon. Such people need a full-fledged rehabilitation course, which often begins already in the hospital. The rehabilitation course itself is prescribed individually, depending on the severity and persistence of the consequences, as well as on the time that has passed since the stroke and general condition patient.
Read about an example of such a rehabilitation center in the article rehabilitation center after a stroke.
Consequences of ischemic stroke

Ischemic stroke(cerebral infarction) is an acute violation of cerebral circulation, as a result of which there is a partial death of brain cells. IN modern world Stroke occupies a leading position among diseases leading to death.
The statistics are disappointing because in the world about 6 million people die from this disease every year. In the first month after the disease, about 30% of people die, and about 50% die within a year. People who managed to survive often become disabled and lose their ability to work.
Ischemic stroke is much more common than hemorrhagic stroke and accounts for 80% of cases. Most often, cerebral infarction affects people in old age, but recently, this disease has become very younger and more and more cases of diagnosing the disease in young people are encountered. There is a chance of complete recovery after mild forms of the disease, but more often the consequences of ischemic stroke remind of themselves throughout life.
Causes of the disease

Development of ischemic stroke
The death of brain cells occurs due to blockage of the vessel responsible for delivering blood to a certain area of the brain, an embolus or thrombus. The presence of a history of pathologies such as arterial hypertension and TIA (transient ischemic attack), doubles the risk of stroke.
Provoking factors can also be:
- Defects of the heart and blood vessels;
- aortic aneurysm;
- Elderly age;
- Hormonal contraception;
- One-sided headache(migraine);
- Bad habits;
- Diabetes;
- Increased blood viscosity;
- The use of trans fats.
If several factors are combined at once, then this is a serious reason to worry about your health, be extremely attentive and know the slightest signs of pathology.
First aid

Ischemic stroke - first aid
To provide first aid, it is necessary to know the initial symptoms of the manifestation of the disease, because not only health, but also human life depends on the correct actions for the first minute of a stroke. If a person becomes ill, then a stroke can be suspected by the following signs:
- Facial asymmetry;
Speech disorder;
To ask a person to raise both hands, he will not be able to do this.
- Put the patient to bed, ensure peace;
- Provide fresh air supply;
- Monitor the state of breathing;
- Prevent tongue slipping;
- Monitor pressure;
- Do not let the patient lose consciousness.
Consequences of ischemic stroke
The consequences of ischemic stroke directly depend on the size of the affected area of the brain and the timeliness of assistance. When assistance is provided in a timely manner and adequate treatment is prescribed, a complete or at least partial restoration of functions is possible. Sometimes, despite the prescribed treatment, the symptoms increase, this can lead to serious consequences.
Headache
Headaches are the most common consequence of ischemic stroke, accompanying the patient throughout life.
Speech disorders

Speech impairment is a common consequence of ischemic stroke. You can recognize a person who has had this disease by his conversation. When the left side of the brain is affected, speech impairment is a typical symptom of the manifestation of the disease.
Speech disorders can manifest as:
- Motor aphasia - characterized by the fact that the patient clearly understands and perceives the spoken speech, but he is not able to form an answer. These patients find it difficult to write and read.
- Sensory aphasia - a person does not perceive the spoken words, and his speech resembles incoherent, illegible phrases. Sensory aphasia greatly affects the emotional state of the patient.
- Amnestic aphasia - the patient's speech is free, but it is difficult for him to name objects.
- The larger the affected area, the worse speech recovery will be. The most active language is restored in the first year after the disease, then the recovery process slows down. The patient must practice special exercises with a speech therapist. Some defects still remain, but a person quickly adapts to them.
cognitive disorders

Cognitive disorders - a decrease in memory, mental capacity for work and other functions. Disorders occur when the temporal lobe is affected.
Depending on the severity of the course, cognitive disorders are divided into:
- Subjective - this form is characterized by such symptoms: impaired attention and memory. Patients do not feel any particular discomfort when subjective symptoms appear.
- Lungs - appear as a deviation from the age norm. Cognitive impairment has little effect on quality of life.
- Moderate - affect the quality of life. The person experiences difficulties in daily life. It takes him a long time to complete simple tasks.
- Severe disorders - a person becomes completely dependent on others. Disorders such as dementia, hysteria and others develop.
This consequence of ischemic stroke develops in 30-60% of cases. Statistics show that disorders in 30% of cases are moderate or mild, 10% are severe disorders.
Impaired coordination

They occur when the lesion is localized in the temporal lobe, because there are centers responsible for the coordination of movements. Depending on the degree of severity, unsteadiness when walking can manifest itself for a long time. To restore coordination, drug treatment is prescribed, aimed at restoring blood circulation in the brain and physiotherapy exercises. Therapeutic massage is highly effective.
Paralysis

Paralysis is a loss or impairment of motor function that affects a specific area of the body. severe consequences of a stroke. When the left side of the brain is affected, paralysis of the right half of the body occurs, with damage to the right hemisphere, paralysis of the left side of the body is noted. If the left side of the body is paralyzed, there is a violation of speech, hearing, vision in the left eye worsens, the motor ability of the left arm and leg worsens.
When the left side of the brain is affected, the right side of the body is paralyzed. The symptoms will be the same as with the defeat of the left side only on the right.
Incontinence
Catastrophic consequences of ischemic stroke for a sick person. The frontal part of the brain is responsible for regulating urination, and when it is damaged, a problem such as urinary incontinence arises. With a high probability, this consequence of a stroke will pass after a few months.
cerebral edema

One of the most severe consequences of ischemic stroke. Fluid accumulates in the tissues and severe headaches appear. Usually, edema occurs immediately after an attack and develops rapidly. Symptoms of complications are vomiting, loss of vision, impaired consciousness, convulsions, headaches, memory loss. A complication in the form of edema can develop into a more severe consequence, such as coma.
Loss or deterioration of vision
Occurs as a complication after the defeat of the occipital lobe. Usually there is a loss of visual fields. The defeat of the right hemisphere leads to loss of visual fields on the left, and vice versa. There are frequent cases of paresis of the muscles of the eye.
Epilepsy
It occurs more often among the elderly. It appears in the form of seizures of varying intensity. Harbingers of seizures are a feeling of anxiety, headaches. During a seizure, if possible, it is necessary to protect a person from unnecessary trauma, turn his head to one side to avoid falling of the tongue.
Swallowing disorder
A common occurrence after a cerebral infarction, in most people, swallowing is restored within a month. But there is a percentage of those people who have residual effects for a long time. This pathology delivers not only discomfort, but can also lead to more serious consequences, such as pneumonia.
Pneumonia

Pneumonia manifests itself in almost 35% of cases. The risk group for pneumonia includes the elderly, patients suffering from chronic diseases, obesity and others. Signs of early manifestation of pneumonia: slight increase temperature, violation respiratory function. The main symptom of pneumonia, such as coughing, may not appear at all, this is due to the suppression of the cough reflex. With untimely diagnosis of pneumonia in the early stages, the symptoms worsen.
Repeated stroke
Recurrent stroke is a typical consequence of a stroke. The occurrence of a second attack is most likely during the first five years after the previous cerebral infarction. If even during the first attack, no consequences appeared, then after the second stroke, the probability of their occurrence is almost 100%.
bedsores
Bedsores - a long stay of the patient in one position leads to complications such as bedsores. To prevent this unpleasant phenomenon, care for a sick person must be thorough.
Thrombosis
With paralysis and prolonged stay in one position, the speed of blood movement slows down and it begins to thicken, which leads to the formation of blood clots. The most likely to form blood clots in the extremities. It is necessary to make as much effort as possible to prevent thrombosis, because it can lead to more serious consequences.
hearing loss
Damage to the temporal lobe of the brain can lead to hearing loss.
Depression after a stroke

Depression after a stroke
Depression after a stroke is a mental disorder characterized by a prolonged decrease in mood. Signs of depression are sadness, lack of desire for life, a negative assessment of oneself and those around them, lethargy. Among patients who have had a stroke, the occurrence of depression reaches 30%. The occurrence of depression is most likely in the case of a severe course of the disease. Scientists have identified such an interesting fact about post-stroke depression, in women the occurrence of this disorder is more likely to occur with damage to the left hemisphere, and in men of the right. The patient is aggressive, irritable, quick-tempered. Concentrating on something, his attention, becomes an impossible task for him. There is sleep disturbance, weight loss, thoughts of suicide.
Drug treatment should be carried out immediately, it can not only protect against unwanted complications, but also save a person's life.
How long do people live after a stroke and possible consequences
A stroke is a terrible pathology that does not pass without a trace. More than 80% of stroke survivors are permanently disabled. Stroke consequences and causes of the disease. How to protect yourself and your loved ones from death and disability. When you need to call a doctor, and what actions to take so that the attack does not cause serious damage to the body.
Description of pathology
What is a stroke? Many of us have heard this name more than once, but each person is sure that this disease will bypass him. Someone thinks that he is too young, others are sure that this is the lot of chronically ill people, and still others believe that this disease can only appear in those who have a hereditary predisposition.

Today, doctors say that yes, indeed, pathology most often affects the elderly and heredity also plays a role, and chronic diseases can cause a stroke. However, experts also argue that no one is immune from this dangerous disease. Increasingly, a stroke overtakes young and at first glance quite healthy people. What is the cause and why is a stroke dangerous?
The cause of a cerebral stroke lies in various vascular diseases. It is the blood vessels that supply the brain with oxygen. Their network is distributed throughout the body, and they must be strong, elastic and clean. If narrowing of the vessel lumen occurs, different reasons, pressure on the wall begins, and it may not withstand and burst. This is how the brain bleeds. Its consequences are most often severe and disrupt important bodily functions.
Another type of stroke is necrosis of brain cells due to blockage of cerebral vessels from oxygen starvation.
The most dangerous stroke with hemorrhage. With a hemorrhage, a hematoma is formed, and it is she who becomes the cause of death and disability of a person. The hematoma grows and compresses the nerve endings that are concentrated in the brain. The brain stops functioning normally. A person may lose speech, motor activity, the ability to breathe independently. The same consequences can develop with necrosis of brain cells, however, ischemic stroke (in which the vessel does not break, but only clogs) is considered the most favorable in terms of prognosis and rehabilitation for the patient.
More about types of stroke
Today, doctors distinguish three main types of stroke. It depends on the type of life expectancy after a stroke and the possibility of maximum recovery after an attack. Types of stroke directly depend on the nature of damage to blood vessels and brain cells, namely:
subarachnoid stroke. The causes of this form of pathology lie in craniocerebral injuries or ruptured aneurysms. Hemorrhage in this case is localized between the soft and arachnoid membranes of the brain. Mortality from this form of pathology is quite high and reaches 50%. However this species pathology is quite rare. Complications after it are the most severe. It develops instantly or within a few hours after the injury.
hemorrhagic stroke. The causes of this form of stroke are rupture of the vessel and hemorrhage in the brain. Mortality from such attacks reaches 33%. However, the degree of disability is very high. In this case, hemorrhage and subsequent hematoma is localized in the ventricles and under the meninges.
An attack of this type develops rapidly and the patient can fall into a coma within a few minutes after feeling unwell.
Ischemic stroke. The attack develops from narrowing or blockage of the vessel. The causes of vasoconstriction vary from atherosclerosis to nervous tension. This is the most common form of stroke. Mortality from it reaches 15%. With timely hospitalization in patients, the prognosis for recovery is most often positive. An attack can develop for several days.
In addition, doctors distinguish an acute type of pathology, a microstroke, an extensive or spinal stroke. All these forms differ in the degree of damage and localization. Forecasts for each individual case are purely individual.
Risk factors
Despite the fact that stroke can develop in any patient nowadays, and even in young people, there are a number of risk factors that are most often present in patients with this diagnosis.
- Age after 50 years.
- The gender is male.
- Heart diseases.
- Arterial hypertension.
- Constant nervous tension.
- Having bad habits.
- The presence of excess weight.
- The presence of diabetes.
- genetic predisposition.
It should be noted that the consequences of a cerebral stroke directly depend on the rate of hospitalization of the patient. Unfortunately, in our country, emergency hospitalization is observed only in 30% of the total number of patients with this diagnosis. Doctors are called when it becomes clear that the situation is critical and the patient is doing very badly. However, for example, an ischemic stroke can develop up to 3 days, and if the patient is taken to the hospital on the first day, his prognosis will be more favorable. Most often, people who lived alone are left without medical help.
Many relatives of patients ask how many years they live after a stroke. There is no single answer to this question. With timely assistance and the implementation of all the recommendations of the doctor, the patient can live for many more years, but it also depends on the age, as well as on the general health of the patient.
Consequences of an attack
A brain stroke invariably leads to negative consequences. In principle, there is no difference between the consequences of a stroke in women and what in men. The consequences of a stroke in men can be observed more often only for the reason that this pathology develops more often in males. The most dangerous complication of a stroke is a recurrent attack.
It is from him that about 40% of patients die in the first 30 days.
The consequences of an attack begin to appear from the first minutes of the impact. The patient experiences the following symptoms, which clearly indicate the development of a cerebral stroke:
- Increasing pressure.
- Increase in body temperature.
- Reaction inhibition.
- Seizures.
- Sharp headache.
- Loss of sensation in one side of the body.
- Loss of orientation.
- Memory loss.
- Speech disorder.
- Coma.
After stopping the attack, the patient may experience the following deviations:
Paralysis. The most common consequence of a stroke is paralysis on one side of the body. Paralysis develops from the side opposite to the localization of the pathology. With this violation, the patient can no longer do without outside help. He needs serious rehabilitation, which can last several years. Basic motor functions should be restored within a year, fine motor skills are restored much longer.
Loss of sensation. This deviation is characterized by a loss of sensation in the muscles of the body. Recovery should be accompanied by exercises to restore motor activity.
With this consequence of a stroke, exercise therapy and other methods of rehabilitation are actively used.
Speech disorders. Recovery of speech skills depends on the specific impairment. Speech problems occur in about a third of stroke patients. A person may experience the following speech problems:
- Impaired understanding of speech.
- Violation of one's own speech.
- Difficulties with the choice of words.
- Violation of both understanding and speech reproduction.
- Complete impairment of speech perception and reproduction.
Recovery of speech functions should begin as early as possible. For this, the patient is recommended special classes with a speech therapist. The recovery time is quite long. As a rule, speech is restored after a few years.
In addition to these consequences, the patient may experience complications such as:
- Muscle hypotension.
- Central pain syndrome.
- Trophic pathologies.
- pathology of vision.
- Difficulties in swallowing.
- Nervous system disorders.
- Impaired coordination.
- Epilepsy.
All these disorders require long-term treatment. Often the care of patients falls on the shoulders of relatives, and it is they who must control the implementation of all the doctor's recommendations. How long people live after a stroke depends largely on the care of relatives. The main task of relatives and doctors is to prevent a recurrent attack and to rehabilitate the patient, which should begin as early as possible.
Recovery forecasts
After a stroke, the prognosis for life is purely individual. Many relatives also want to know when a complete recovery of the patient is possible. Doctors say that rehabilitation is influenced by many factors, including the desire of the patient himself. The most favorable forecasts for recovery are predicted under the following factors:
- Young age.
- early hospitalization.
- Stroke of moderate and mild severity.
- Localization of stroke in the vertebral arteries.
- Complete care.
- Properly organized rehabilitation.
Forecasts for life
Survival forecasts are the main thing that relatives expect from doctors when they close person is admitted to the hospital with a stroke. Stroke how long do they live after an attack, and what does this prognosis depend on? Most often, doctors do not give specific predictions. The main thing, they say, is to prevent a second attack within 30 days. Then a person must live for a year, and only after this period the risk of death gradually decreases.
Recurrent stroke is the most common cause of patient death.
The following factors influence the development of a relapse:
- Patient's age.
- Late admission to the hospital.
- The presence of chronic diseases before the attack.
- Poor quality care.
- Failure to follow the recommendations of doctors.
- Stress and nervous tension.
Doctors say that if negative factors are excluded as much as possible and a competent approach to the treatment and rehabilitation of the patient, the prognosis for life can be favorable. Some patients live a long life, gradually recovering and learning to live again. Of course, there are more chances to survive at a young age, but even older people sometimes show such a desire to live that it surprises even doctors.
Thus, it can be argued that the predictions depend on how much the brain has been damaged, on the patient's age, care for him and his desire to live. It is with the last point that problems often arise. Elderly people do not want to fight, they do not want to become a burden for their relatives. In this case, you need to consult psychologists and support relatives. Only by reviving the desire to be healthy in a person, you can count on his speedy recovery.
Stroke is a very scary and serious disease. Very often, a stroke ends in death or leads to disability. The result of the disease depends on how quickly and efficiently assistance will be provided during the illness. A stroke can damage different parts of the brain. After a stroke, vision, speech, movement, or coordination may be impaired.
The term "coordination" comes from the Latin coordination - mutual ordering. Under the coordination of movements understand the processes of coordination of the activity of the muscles of the body, aimed at the successful implementation of the motor task.
Development of coordination of movements of the child early age is an extremely important factor in its development as a whole. physical training, improving the dexterity of movements, mobility, rhythm of the child will be facilitated by the performance of simple and interesting tasks that the mother can come up with herself.
What is needed to carry out active classes? Balls, balls, jump ropes, rubber bands, skittles, spoons, small toys, hoops, gymnastic sticks - all this and more will come in handy. It is desirable that the balls and sticks are of different colors - then in the process of completing the task, you and your baby will be able to pay attention to the colors. In addition to balls, you can use various durable objects (made of wood) to study a specific topic, for example, the topic "Transport" - cars, "Food" - plastic vegetables and fruits.
How can the above items be used in children's games? We offer you the following exercise options, but first - short recommendations for parents.
One game should last no more than 5-7 minutes.
When starting the game, show the child how to play (where to get the ball, where to put it, how to pass the "obstacle course").
Perform all game active exercises to cheerful children's music. If the child is from one to two years old, it is advisable to use the same song in games so that the baby learns to differentiate the time for games from other developmental tasks.
Accompany a child 1-2 years old in the game: step by step complete the task together.
End the lesson whenever you see that the child is tired.
Development of coordination of movements. Games
The human body is the most complex system imaginable. So, for the implementation of any simple movement, the brain, many nerve endings, joints, ligaments and muscles are simultaneously involved. Impaired coordination of movement indicates that an “error” occurred in the transmission of a signal from the brain to the muscles. Similar problems can be observed in both children and adults, they occur if there are disorders of the central nervous system (CNS), which includes nerve cells in the brain and spinal cord.

There are various causes of incoordination, including:
- parkinsonism (damage to the central nervous system, accompanied by a decrease motor ability person);
- stroke and other neurological diseases;
- physical exhaustion of the body and muscular dystrophy;
- diseases of the musculoskeletal system;
- poisoning of the body with alcoholic, narcotic and other psychoactive substances, as well as drugs;
- age and sclerotic changes;
- brain injury;
- catalepsy (a painful condition in which a person seems to “freeze” in one position).
If we talk about impaired coordination of movement in children, then this can be caused by injuries (including birth), infectious diseases and inflammatory processes, intoxication of the body, as well as hereditary diseases of the nervous system.