Sports medicine pathology. Irina Gretskaya course of lectures on sports medicine for self-study of part-time students
Sport, in the broad sense of the term, is a competitively organized physical or mental activity of people. Its main goal is to maintain or improve certain physical or mental skills. In addition, sports games are entertainment, both for participants in the process and for spectators.
The concept of pathogenesisGeneral pathology is theoretical background clinical medicine. The subject of study of general pathology are the most common causes and patterns of occurrence, development and course of diseases.
Pathogenesis is the study of the mechanisms of development, course, individual characteristics and outcome of diseases.
Pathogenesis answers the question: how does the disease develop?
There are general and particular pathogenesis.
General pathogenesis is a section of general nosology devoted to the development of ideas about the general patterns of development of diseases and pathological processes and the substantiation of the principles and methods of their pathogenetic treatment and prevention. Nosology is the general study of disease.
Private pathogenesis - is used to refer to the mechanism of development of a particular disease or a particular pathological process.
Pathogenetic factors are exclusively internal factors (physiological and pathological) that determine the development of the disease.
Pathogenetic factors of the disease are those changes in the body that occur in response to the action of the main etiological factor and in the future, even in its absence, determine the development of the disease.
Allocate the main pathogenetic factor, without which the development of the disease is impossible. Treatment aimed at eliminating the main pathogenetic factor is called pathogenetic, it leads to the recovery of the body.
With the development of any disease, specific and non-specific mechanisms of its development are distinguished.
The primary and main processes in the development of any disease are damage, destruction, disorganization of the structures and functions of the diseased organism.
In the development of the disease, local and general changes are distinguished. It must be emphasized that there are no absolutely local processes in the whole organism. In almost any local pathology (for example, pulpitis, furuncle), the entire body is involved in the pathological process. The role of local and general processes in pathogenesis is different.
Local and general disorders during illness mobilize various defense mechanisms aimed at eliminating functional and structural disorders, restoring the constancy of the internal environment of the body.
In illness, there are always various protective, adaptive and compensatory reactions that contribute to recovery.
Protection mechanisms include:
- Protective reactions of the body are physiological, biochemical and morphological reactions (reflex, humoral) that occur in response to the action of stimuli that are harmful or damaging in nature. These reactions are the product of evolutionary development and have non-specific properties.
- adaptive processes.
All protective, adaptive processes are always secondary, developing after damage when exposed to pathogenic factors on the body. Adaptive reactions develop in response to disorders that occur during illness and ensure the unity of the organism with the external environment at a new level of its vital activity.
Distinguish between active and passive devices:
- Active adaptation is the mobilization of the most important life-supporting systems and functional reserves that ensure adaptation; it is characterized by a high level of vital activity of the organism.
- Passive adaptation occurs when the body cannot provide an energetically active adaptation in response to the action of pathogenic factors (large blood loss, severe trauma, etc.). At the heart of passive adaptation lies the transcendental, protective inhibition of the central nervous system, in which the existence of a diseased organism is ensured by a sharp decrease in its energy consumption. 3. Compensatory mechanisms.
Compensatory mechanisms are activated with persistent dysfunction.
Compensatory processes are the most important part of the body's adaptive response to damage, which is expressed in the fact that organs and systems that are not directly affected by the action of a damaging agent take on the function of damaged structures through substitutional hyperfunction or a qualitatively altered function.
In its development, compensatory processes have two stages: the stage of urgent compensation and the stage of long-term compensation.
Compensatory mechanisms are functional compensation:
- mobilization of functional reserves that ensure adaptation, i.e. the inclusion of reserve stocks of the diseased organ, and
- hyperfunction, i.e. increase in the intensity of the work of organs and tissues.
The emergence of only functional compensation does not provide stable adaptation to the action of a damaging factor. If the resulting hyperfunction of any organ or system is sufficient to eliminate the defect that has arisen, then the compensatory process may be limited to this. This is immediate compensation.
Long-term compensatory hyperfunction of organs leads to the formation of appropriate structural changes.
There are the following structural compensations:
- a) hypertrophy;
- b) hyperplasia;
- c) regeneration (the process of restoring an organ and tissue after damage);
- d) compensatory deformation;
- e) the development of collaterals in violation of blood flow in the main vessels that feed the organ.
In the process of compensation, structural changes occur not only in the cells of the executive organ, which has an increased load, but also in all parts of the compensatory system. This is the basis for the transition from urgent adaptation to long-term adaptation.
It should be noted that in the process of development of any disease, adaptive and compensatory processes can become harmful to the patient and seriously affect his condition. For example, severe and prolonged fevers.
The concept of heredityGenetics is a science that studies the phenomena of heredity and variability of the human body.
Heredity is the property of organisms to preserve and pass on to the next generation inherent given organism features of the structure and development.
Variation is a phenomenon that ensures natural selection in evolution, due to which new characters appear in offspring.
Medical genetics studies the role of heredity in pathology, patterns of transmission of hereditary diseases, methods of diagnosis, prevention and treatment of hereditary diseases, as well as diseases with a hereditary predisposition.
Chromosomes are the material basis of heredity. A gene is an elementary particle of a chromosome, a unit of structural and functional heredity. A gene is a specific section of DNA that carries information in the form of a genetic code. The genotype is not just the sum of genes, but a highly organized system of interacting elements.
Hereditary diseases are human diseases caused by chromosomal or gene mutations.
All hereditary diseases are divided according to the nature of the change in hereditary structures into 3 main types of disorders:
Genetic diseases are mutations of individual genes.
Chromosomal diseases are abnormalities in the number or structure of chromosomes.
Diseases with a hereditary predisposition (their manifestation requires the combined action of heredity and environmental factors).
Chromosomal diseases:
- Down's disease;
- Shershevsky-Turner syndrome, etc.
Genetic diseases include numerous metabolic diseases:
- cystic fibrosis;
- Marfan syndrome;
- Ehlers-Danlos syndrome, etc.
The processes of human adaptation to environmental conditions are closely related to heredity, it is inseparable from the body as a whole, ensuring the stability of vital functions to preserve and maintain life at any level of balance.
The concept of reactivity and resistance1. Reactivity is the ability of an organism to adequately respond to changing conditions of the external and internal environment.
There are individual and group reactivity:
- a) individual reactivity - these are the features of the response of each person to the action of factors of the external and internal environment;
- b) group reactivity is reactivity individual groups people united by some common feature, on which the characteristics of the response of all representatives depend
of this group on the impact of the external environment. These features include age, gender, type of constitution, etc. The main form of group reactivity is constitutional.
Physiological and pathological reactivity are also distinguished:
- a) physiological reactivity - these are forms of response to the action of environmental factors without disturbing the body's homeostasis;
- b) pathological reactivity - these are forms of response to the action of environmental factors that violate the body's homeostasis.
Homeostasis is the relative dynamic constancy of the internal environment (blood, lymph, tissue fluid) and the stability of the main physiological functions the human body (blood circulation, respiration, thermoregulation, metabolism, etc.).
It depends on the reactivity of the organism whether or not a disease occurs under the action of a pathogenic factor and how the disease will proceed.
There are specific and non-specific reactivity:
- a) specific (immune) reactivity - this is the body's ability to respond to the action of an antigen by producing antibodies, i.e. specific immune response;
- b) non-specific reactivity is a complex of changes in the body that occur in the body in response to external factors and are not associated with the immune response. For example, changes in the body in response to hypoxia.
Reactivity is not a quantitative concept. In different age periods, people react differently to the same influences. Each age has its own characteristics and a tendency to develop certain diseases. Particular reactivity is characteristic of children and the elderly.
Early childhood is characterized by reduced reactivity and resistance, which is due to the incomplete development of the nervous, endocrine and immune systems, immaturity of enzyme systems, imperfection of external and internal barriers.
In early childhood:
- there is an insufficient manifestation of protective-adaptive and compensatory reactions, there is a tendency to generalized reactions and the development of complications in infectious diseases;
- the formation of heat regulation mechanisms has not been completed (overheating and hypothermia easily occur);
- resistance to hypoxia is observed.
During puberty, there is an excessive instability of the autonomic nervous system, psyche, behavior. Possible violations of the cardiovascular system (juvenile hypertension). Deviations from the norm of the process of sexual development are possible (it can be accelerated or, conversely, slowed down).
As the body grows, tissue barriers and the immune system develop and improve, and neuroendocrine regulation improves. Therefore, in people of mature age, reactivity and resistance are most pronounced. The same is observed in the development of protective-adaptive and compensatory reactions, which contributes to a favorable outcome of diseases. Thus, the optimal for the vital activity of the organism is the reactivity in adulthood when all systems are formed and function fully.
When moving from mature to old and senile age, a decrease in reactivity and resistance is again observed. The aging process is characterized by the development of structural and functional changes that limit the body's ability to maintain homeostasis, which leads to increased morbidity:
- the ability to adapt to the effects of changing physiological and pathological environmental factors decreases due to a decrease in metabolism and functional reserves of various organs;
- there is an inhibition of immunological reactivity, anti-infective decreases. Therefore, diseases caused by viruses and bacteria are especially common, which is associated not only with insufficient formation of antibodies, but also with a weakening of the activity of phagocytes and an increase in the permeability of tissue barriers;
- antitumor resistance decreases (this is facilitated by the weakening of immune surveillance);
- the frequency of cardiovascular pathology increases due to the development of atherosclerosis;
- increased incidence of diabetes mellitus;
- dementia develops (senile dementia);
- increased frequency of bone fractures due to the development of osteoporosis;
- diseases have a chronic course and are often characterized by insufficiently clear manifestations due to a decrease in reactivity.
The reactivity of the body is associated with sex. In the female body, reactivity changes in connection with the menstrual cycle, with pregnancy, with the menopause. Female reactivity provides greater vitality in relation to a variety of natural exogenous factors.
2. Resistance is the body's resistance to the effects of various damaging factors. Resistance is closely related to reactivity.
Resistance is a quantitative concept that reflects the degree of resistance of an organism to a particular pathogenic factor. It cannot be universal due to differences in the nature of pathogenic factors.
Factors of natural resistance (stability). There are a number of non-specific protective factors:
- a) the barrier role of the integument of the body (barrier functions are functions carried out by special physiological mechanisms (barriers) to protect the body or its individual parts from environmental changes and preserve the relative constancy of the composition, physicochemical and biological properties of the internal environment (blood, lymph, tissue fluid));
- b) mechanical reliability of the musculoskeletal system;
- c) a system of phagocytes, including neutrophils and macrophages;
- d) interferons;
- e) substances involved in inflammatory reactions, some of them have a direct bactericidal effect.
The immune system. Types of immunity
Immunity is the body's immunity to infectious and non-infectious agents and substances that have foreign (antigenic) properties.
The immune system protects the body from infections, removes damaged, aged and altered cells of its own body.
The main function of the immune system is to distinguish genetic foreign structures from its own, process and remove them, and remember, which leads to an accelerated response to repeated exposure to the same agents. Specificity and memory are the two main hallmarks of an immune response. Upon repeated exposure to an antigen, the immune system is able to respond more effectively than upon initial exposure to the same antigen.
Antigen-recognizing cells are T-lymphocytes and B-lymphocytes. All lymphocytes are derived from bone marrow stem cells, but T lymphocytes then develop in the thymus and B lymphocytes develop in the bone marrow. T-lymphocytes carry out the cellular immune response, which plays a role in creating protection against intracellular agents, such as viruses. B-lymphocytes are responsible for the humoral response aimed at defeating extracellular infectious agents.
The immune system eliminates infectious agents and minimizes the damage they cause. Thanks to the immune system, most infections are short-term and do not leave undesirable consequences for the body.
The organs of the immune system are divided into central and peripheral.
1. The central organs of the immune system are:
- thymus gland (this is the central lymphoid organ);
- (central lymphoid organ).
2. Peripheral organs of the immune system are:
- (peripheral lymphoid organ, the main site of antibody formation, the main arena for the destruction of cells - both microbial and own. "The spleen is a graveyard of erythrocytes");
- (peripheral lymphoid organ, lymph nodes work as filters in the lymph circulation system);
- tonsils (accumulation of lymphoid tissue in the thickness of the mucous membrane at the border of the nasal, oral cavities and pharynx);
- lymphoid tissue;
- blood is a component of the immune system (the blood system is peripheral blood, hematopoietic and blood-destroying organs (bone marrow, liver, spleen and lymph nodes)); peripheral blood is blood plasma and the formed elements (erythrocytes, leukocytes and platelets) that are in suspension in it.
There are two main types of immunity:
- a) congenital
- b) purchased.
Congenital includes species immunity and immunological features due to heredity.
Acquired is divided into natural and artificial, and each of these types is divided into active and passive.
Natural active immunity occurs as a result of an infection. Natural passive immunity is due to antibodies received by the child from the mother (during the prenatal period and during breastfeeding).
Artificial active immunity occurs after vaccination. Injected vaccines contain antigens (killed or weakened microbes) for which the body actively produces antibodies.
Artificial passive immunity occurs after the introduction of serum containing antibodies.
Active immunity persists for a long time, for years, passive - for a short time.
- a) is provided by T-lymphocytes and B-lymphocytes; they are responsible for the specific recognition of antigens. Specific immune recognition of pathogenic microorganisms is a function of T-lymphocytes and B-lymphocytes, therefore, it is these cells that initiate the immune response;
- b) humoral immunity is due to the presence of antibodies (immunoglobulins) in body fluids - blood, lymph, tissue fluid.
Immunoglobulins (antibodies) are plasma proteins.
Immune system disorders
All violations of the functions of the immune system are divided into 3 groups:
- Immunological deficiency is a congenital or acquired defect of the immune system, which is expressed by the inability of the body to carry out reactions of cellular and (or) humoral immunity.
- is an ineffective immune response. If a defect occurs in any elements of the immune system, then the body's defense against infections becomes inadequate, and immunodeficiency occurs.
- Hypersensitivity (allergies).
Hypersensitivity is a consequence of an excessively high immune response. Immune responses can sometimes exceed the response needed to fight a foreign agent. For example, the response of the immune system to food antigens that are harmless to the body. Such inadequate reactions can cause even more severe damage than the microorganisms themselves or their antigens.
Autoimmunity.
Autoimmunity results from a reaction to self antigens. Under normal conditions, the immune system recognizes all foreign antigens and responds to them as foreign, and recognizes its own antigens as its own and there is no response to them. The survival of a macroorganism is closely related to the unique ability of the immune system to distinguish between “self” and “non-self”.
In the case of a reaction of the immune system against "their own" (own antigens), an autoimmune disease occurs. Autoimmune mechanisms underlie many systemic diseases.
The concept of immunodeficiencyImmunodeficiency is a violation of immunological reactivity. Distinguish between primary and secondary immunodeficiency:
- primary (hereditary) - not associated with any diseases or extreme exposure, manifests itself shortly after birth;
- secondary (acquired) - due to any other diseases or extreme effects, develops during life.
Secondary immunodeficiency occurs:
Immunodeficiency diseases are diseases caused by a congenital or acquired defect in the immune system, characterized by the body's inability to carry out cellular and (or) humoral immunity reactions.
The concept of allergiesAllergy is a specific hypersensitivity of the body to various antigens (allergens), associated with changes in its reactivity. Allergy is a typical immunopathological process.
Allergy is a problem of an organism that is genetically predisposed to an unusual reaction to an antigenic irritant that is common for many other individuals, and not a consequence of the evil nature of the allergen itself.
Allergy or hypersensitivity is a phenomenon based on typical immunological processes that develop in a sensitized organism in the mode of a secondary immune response upon contact with an antigen that caused sensitization, resulting in inflammation.
Sensitization is the primary immune response to an allergen.
Allergens are antigens that provoke an allergy.
Allergens are divided into:
1. Exogenous (external), entering the body from the external environment.
Exogenous (external) allergens by origin are infectious and non-infectious:
- infectious allergens include bacteria, viruses, fungi and their metabolic products;
- non-infectious allergens include household, food, pollen, epidermal, medicinal.
Exogenous allergens can enter the body through the skin, Airways, gastrointestinal tract, blood.
2. Endogenous (internal), existing or formed in the body itself.
Endogenous (internal) allergens or autoallergens are divided into:
- primary (natural);
- secondary (acquired).
Primary (natural) autoallergens are antigens contained in the "beyond the barrier" organs and tissues (in the lens of the eye, colloid of the thyroid gland, gray matter of the brain, testes), which in the process of evolution turned out to be isolated from the apparatus of immunogenesis. With an increase in the permeability of barriers, autoantigens are released from these organs and tissues and contact with the immune system - the production of autoantibodies begins, which interact with autoantigens and, as a result, damage to these organs and tissues occurs.
Secondary (acquired) non-infectious autoallergens are formed from their own proteins under the influence of various factors (ionizing radiation, exposure to high and low temperatures, organ ischemia). On them, the body produces autoantibodies. This is of great importance in the pathogenesis of radiation and burn diseases.
Secondary (acquired) infectious autoallergens are formed from their own proteins under the influence of microorganisms. This is of great importance in the pathogenesis of infectious-allergic myocarditis and infectious-allergic bronchial asthma.
Allergic reactions are clinical manifestations of increased sensitivity of the body to various antigens.
All allergic reactions according to the timing of the appearance of the first symptoms in response to the allergen entering the sensitized organism are divided into two groups:
- a) immediate type (rapid development after contact - within a few minutes);
- b) delayed type (symptoms appear 4-6 hours after contact with the antigen and increase within 1-2 days, reaching a maximum severity).
If allergic reactions are directed to autoantigens, then they speak of autoallergic reactions, which can lead to autoimmune diseases.
Autoallergic diseases are a group of diseases, the main mechanism of which is the reaction of autoantibodies and sensitized lymphocytes with their own tissues.
Features of the immune system of athletesIt has now been established that with a properly selected, adequate training regimen, the activity of the immune system increases, while the body's resistance to various infectious diseases and other adverse environmental factors increases. The process of increasing fitness to a certain limit is associated with an increase in nonspecific resistance of the body of athletes. With a further increase in fitness, a disconnection gradually arises between fitness and nonspecific resistance, when the increase in fitness no longer entails an increase in the body's nonspecific resistance.
At the same time, it has been proven that inadequate physical activity, including competitive ones, is accompanied by an increase in the incidence of infectious diseases. This growth is based on a decrease in the immunological reactivity of athletes under the influence of excessive physical activity. Prolonged stress, including stress caused by physical and emotional overload, can dramatically weaken the immune system.
A decrease in the body's defenses against the background of irrational (in magnitude and intensity) loads can take the form of both acute diseases and exacerbation of chronic diseases, as well as the appearance of allergic reactions or allergic diseases.
Also, the tension of the immune system in an athlete against the background of physical activity is possible under the following conditions: dysbacteriosis, allergies, foci of chronic infections, acute infections, temporary desynchronosis.
It should be noted that even moderate physical activity in combination with a stressful situation causes a decrease in immunity.
A number of studies conducted over the past decades in Russia and abroad have shown that elite sport has a depressing effect on the immune system. Almost all athletes are at risk for the development of immunological deficiency. Significant immunological deficiency occurs in 40% professional athletes.
The results of the analysis of the incidence of young athletes in general, compared with schoolchildren, indicate that the incidence of athletes with acute respiratory infections (rhinitis, nasopharyngitis, pharyngitis, laryngitis, tonsillitis, tracheitis, bronchitis) is much higher.
It has been established that an intense training load when bringing to the "peak" of sports form and maintaining high sports performance at the "peak" of sports form can dramatically reduce the immunological reactivity of an athlete. As a result, athletes at the peak of their sports form sharply increase the frequency of acute and exacerbation of chronic diseases, which naturally reduces their athletic potential and the ability to achieve high results. Immune system disorders are a factor limiting the performance of an athlete.
Typical pathological processA pathological process is a natural sequence of phenomena, including protective and adaptive reactions and life disturbances in various combinations under the influence of a pathogenic factor.
Typical pathological processes are the same type of processes that occur in response to the influence of various damaging factors.
Typical pathological processes have developed evolutionarily and are genetically programmed, they are stereotyped, universal, polyetiological.
Typical pathological processes include:
- peripheral circulatory disorders;
- inflammation;
- fever;
- necrosis;
- atrophy;
- hypertrophy;
- tumors;
- metabolic disorders in tissues.
The same pathological process, caused by various etiological factors, is a component of various diseases and at the same time retains its distinctive features.
For example, inflammation can be caused by the action of mechanical, physical, chemical, biological factors. Taking into account the nature of the causative factor, the conditions of occurrence and the response of the body, it is very diverse, however, despite this, in all cases, inflammation remains a holistic, standard response to damage.
The concept of inflammationInflammation is a typical pathological process. Inflammation is a complex complex local vascular tissue protective and adaptive reaction of the whole organism to the action of a pathogenic stimulus. Causes of inflammation:
Morphological signs of inflammation:
a) alteration is a change in the structure of cells, tissues and organs, accompanied by a violation of their vital activity.
Alteration can be considered as a result of the direct action of the pathogenic factor and metabolic disorders that occur in the damaged tissue. This is the first phase of inflammation.
Alteration is necessary to destroy the damaging agent;
b) exudation is a violation of blood circulation and permeability of the vascular wall with the release of the liquid part of the blood into the tissues, containing various fractions of proteins and uniform elements. The fluid formed during inflammation is called exudate. Exudation plays a central role in the barrier function of the organism;
c) proliferation is the reproduction of tissue elements, restoration and replacement of a tissue defect due to connective tissue.
A scar is a section of connective tissue that replaces a defect in the skin, mucous membrane, organ or tissue that has arisen as a result of their damage or pathological process. The process of scar formation is called scarring and is a manifestation of regeneration.
Regeneration is the renewal of body structures in the process of life and the restoration of those structures that were lost as a result of pathological processes.
Sclerosis is a hardening of an organ due to the replacement of its dead functional elements with connective tissue.
Meaning of inflammation:
Inflammation is the body's emergency defense system. Inflammation is a biological and mechanical barrier, which ensures the localization and destruction of the damaging agent and the tissue damaged by it, as well as the restoration of damaged tissue or the replacement of a tissue defect.
Inflammation also performs a drainage function (with exudate from the blood, products of impaired metabolism, toxins come out to the inflammation site).
Inflammation affects the formation of immunity.
Inflammation as a local process with a certain localization and prevalence may be accompanied by general pathological manifestations (fever, leukocytosis). General reactions in inflammation are based on a protective or adaptive orientation. But with excessive severity (intoxication, changes in reactivity, etc.), they can harm the body.
The concept of feverFever is a non-specific systemic typical pathological process characterized by active retention of heat in the body due to a shift to a higher level of the "setting point" of the center of thermoregulation under the influence of pyrogenic factors.
Fever is part of the mechanisms of innate immunity.
Fever is a polyetiological process, that is, caused by various reasons. The cause of fever is most often infectious diseases, but can also be non-infectious, for example, cancer.
The essence of fever is the reconfiguration of thermoregulation mechanisms to a higher level of functioning. During fever, the increase in body temperature does not depend on the ambient temperature, the mechanisms of thermoregulation during fever are preserved.
Fever is basically an adaptive reaction that increases the body's resistance to infectious diseases.
Thermometry is a method of measuring body temperature. The readings are recorded on a temperature sheet and, on the basis of marks made over several days, a temperature curve is obtained, which has a characteristic appearance in many diseases.
Usually the temperature is measured 2 times a day (at 7-8 o'clock and at 17-19 o'clock). The normal temperature when measured in the armpit is 36.4-36.8 C.
During a fever, there are:
1. Temperature rise period.
The degree of temperature increase largely depends on the state of the patient's body; with the same infection in different individuals, it can be different.
With an increase in temperature by one degree, the intensity of metabolic processes increases by 12-15%.
A rapid and significant increase in temperature is usually accompanied by chills. With chills, the blood vessels of the skin narrow, the skin turns pale, the patient feels very cold, trembles.
Chills is one of the reactions of enhanced thermogenesis, manifested by muscle tremors and a feeling of cold, which develops in patients as an integral part of the febrile reaction.
2. Period of high temperature.
At high body temperature, the skin turns red, becomes warm, the patient feels hot.
The degree of temperature rise: - 37-38°C - subfebrile;
Subfebrile condition is a constant increase in body temperature ranging from 37.1 to 38 ° C, noted for a long time, from two weeks to several months or years. Subfebrile condition is a non-specific reactive state of the body that occurs with various diseases and is associated with a temporary restructuring to a higher level of heat exchange regulation.
Subfebrile condition is distinguished: low - with a temperature of 37.5-37.5°C and high - with a temperature of 37.5-37.9°C.
- 38-39° - moderately elevated;
- 39-4°° - high;
- 4°-41° - excessively high;
- 41-42° - hyperpyretic.
Temperature drop period.
The decrease in temperature can occur gradually - over several days, or quickly - the temperature drops to normal within a day. A rapid drop in temperature is accompanied by profuse sweating.
Fever Meaning:
- a) an alarm signal (sometimes this is the first and only sign of a disease);
- b) creates a temperature optimum for metabolic and recovery processes;
- c) enhances the body's immune response;
- d) increases antibacterial and antiviral specific and nonspecific protection.
The negative effect of fever on the body:
- a) with a pronounced and prolonged increase in temperature, cardiac function is stimulated, which can lead to the development of an overload form of heart failure in the elderly and patients with heart disease;
- b) the possibility of developing collapse with a critical drop in body temperature;
- c) with a high fever, suppression of immune responses may occur;
- d) at high temperatures, children may develop convulsions and swelling of the brain or acute circulatory failure.
Leukocytes are the formed elements of the blood (white blood cells). The functions of various leukocytes are varied. Leukocytes carry out the following functions:
- protective;
- detoxification;
- prevent the development of allergic reactions;
- play an important role in the formation of immunity.
Leukocytosis is an increase in the number of leukocytes in the peripheral blood. This is a non-specific protective-adaptive reaction. Leukocytosis is determined in the blood in any pathological process first of all, since leukocytes in the first hours of inflammation are mobilized from their depots and enter the blood (therefore, their number in the blood increases) and quickly migrate to the focus of inflammation (they are able to actively move, leave the bloodstream and move to the source of damage).
The protective and adaptive effect of leukocytosis consists in the destruction of substances foreign to the body - microbes, toxins, pathologically altered own proteins. Leukocytes are involved in the regeneration (recovery) of tissues.
Leukocytosis is an alarm signal, gives an idea of the severity of the disease and its dynamics, allows you to determine the presence of complications of the disease.
The concept of hypertrophyHypertrophy is an increase in the volume of organs, tissues, cells while maintaining their configuration.
There are the following types of hypertrophy:
- false hypertrophy is an increase caused by the growth of interstitial tissue in the organ, often fatty, while the active part - the parenchyma - does not increase in volume, but often decreases (atrophies) and the function of the organ decreases;
- true hypertrophy is an increase in the volume of the constituent parts of the organ, its parenchyma due to the functional load.
True hypertrophy:
- working occurs with increased work of the body. In conditions of sports activity, it is the result of adaptation (an increase in the volume of the heart and skeletal muscles). In conditions of pathology, it develops as a compensatory phenomenon (for example, cardiac hypertrophy with heart defects). With pronounced hypertrophy, decompensation may occur, i.e. weakening of the organ function up to its complete cessation;
- vicarious hypertrophies occur in one of the paired organs (for example, kidneys, lungs), when one of them ceases to function, and the remaining organ increases in volume.
Atrophy is a lifetime decrease in the volume of organs, tissues, cells, accompanied by a weakening or cessation of their function.
Distinguish between physiological and pathological atrophy:
- physiological - after birth, the umbilical arteries atrophy and overgrow, in older people the skin becomes thinner and loses its elasticity;
- pathological - more often caused by malnutrition, impaired blood supply, the activity of the central and peripheral nervous system, the activity of the endocrine glands.
The main mechanism for the development of atrophy is an insufficient supply of nutrients to the organ.
Pathological atrophy is divided into:
- dysfunctional (for example, muscle atrophy due to bone fractures and joint diseases);
- due to insufficiency of blood supply (atrophy of brain tissue in atherosclerosis of the cerebral vessels).
Atrophy is a reversible process and at a certain stage, when the cause that caused the atrophy is eliminated, it is possible to restore the structure and function of the atrophied organ.
The concept of dystrophyDegeneration of cells and tissues is a pathological process that occurs in connection with a metabolic disorder and is characterized by the appearance in cells and tissues of metabolic products that have been changed quantitatively or qualitatively.
Cellular dystrophies are metabolic disorders accompanied by a disorder in the function of cells, plastic processes in them, as well as structural changes leading to disruption of cell activity.
Metabolism is the basis of the life of the organism, an essential and indispensable sign of life. The essence of metabolism lies in the totality of physiological and biochemical reactions that take place in living organisms, including the assimilation of organic and inorganic compounds from the external environment (assimilation) and their splitting (dissimilation) up to the formation and release of end products of metabolism.
The main factor in the development of dystrophic processes are trophic (nutrition) disorders.
Trophics is a set of nutrition processes for cells and non-cellular elements of various tissues that ensure growth, maturation, preservation of the structure and function of organs and tissues and the whole organism.
Causes of dystrophies:
- energy deficiency and violations of enzymatic processes in the cell;
- hypoxia;
- disorders of neuroendocrine regulation of trophism.
Dystrophy mechanisms:
- a) the synthesis of abnormal substances that are not normally found in the cell;
- b) excessive conversion of some compounds into others;
- c) disintegration of structures and substances, decomposition;
- d) infiltration of cells and intercellular substance with organic and inorganic compounds.
The main criteria for the classification of cellular dystrophies are predominantly metabolic disorders of certain classes of substances. According to this, dystrophies are distinguished:
- protein,
- carbohydrate,
- fatty,
- mineral.
Dystrophies can be general and local.
The concept of tumorsA tumor is a typical pathological process, which is based on unlimited, uncontrolled cell growth with a predominance of proliferation processes over the phenomena of normal cell differentiation (Ado A.D.).
Tumor formula: "plus growth, minus differentiation."
The main etiological factors in the development of tumors are carcinogens. They have mutagenic activity and cause changes in the genetic apparatus of the cell.
Carcinogenic factors are divided into:
- a) exogenous;
- b) endogenous.
Exogenous carcinogenic factors are:
- physical (ionizing radiation, UFL - radiation, thermal effects, mechanical injuries);
- biological (viruses - adenoviruses, herpes viruses, retroviruses);
- chemical (aromatic azo compounds, asbestos, nitroso compounds, metals - nickel, cobalt, chromium, arsenic, titanium, zinc, lead, iron).
There are benign and malignant tumors:
Benign tumors have expansive growth, as a result of which the surrounding tissues are retracted or moved apart, sometimes compressed and subjected to atrophic changes.
Benign tumors, as a rule, do not leave the tissue of the organ in which they have developed, and do not invade neighboring organs. After surgical removal of a benign tumor, it ceases to exist.
Malignant tumors are characterized by infiltrating growth (going beyond the original tissue, germination into the surrounding tissues). Infiltrative (invasive) growth is the main criterion that distinguishes malignant tumors from benign ones. Malignant tumors are also characterized by the ability to metastasize. During the period of rapid growth of a malignant tumor, immature cells appear, characterized by tissue and cellular atypism.
Atypism is a set of characteristic features that distinguish tumor tissue from normal tissue and make up the biological characteristics of tumor growth.
Cells of malignant tumors can detach from the main focus and spread throughout the body by lymphogenous and hematogenous routes, settling in distant organs and forming secondary foci of tumor growth (metastases) there. One of the important properties of a malignant tumor is autonomy in unlimited growth and tumor progression - the continuous evolution of the tumor towards an increasingly aggressive and uncontrolled tissue. After surgical removal of the tumor, it is characterized by a recurrence of the tumor process (this can be in the form of a local appearance of a tumor at the site of the remaining invisible micrometastases or in the form of distant metastases).
There are 3 ways of metastasis of a malignant tumor:
- hematogenous - through the blood vessels;
- lymphogenous - through the lymphatic vessels;
- tissue - directly from one adjacent tissue to another or through interstitial spaces.
Malignant tumors:
- from epithelial tissue are called "cancer", "cancer", "carcinoma";
- from connective tissue - sarcoma;
- tumors of hematopoietic and lymphoid tissue - hemoblastosis (for example, leukemia is a tumor arising from hematopoietic cells with obligatory damage to the bone marrow and displacement of normal hematopoietic sprouts).
Malignant tumors are the second leading cause of death after cardiovascular diseases. Unfortunately, tumors are found in all age groups, both in women and men, and are detected in almost all organs and tissues. Malignant tumors often lead to lethal outcome, sometimes in a relatively short time, all this is aggravated by physical suffering associated with pain, cachexia, dysfunction of a number of organs, especially with tumor metastasis.
Cancer cachexia is a state of general exhaustion of the body.
Arterial hyperemiaHyperemia is an increase in blood supply in any part of the peripheral vascular system (small arteries, capillaries and veins), caused by an increase in blood flow to the microcirculatory system (arterial hyperemia) or a weakening of blood outflow (venous hyperemia).
Arterial hyperemia is an increase in the blood filling of an organ as a result of excessive blood flow through the arterial vessels. This process is also called active hyperemia, since the arteries and arterioles expand during dynamic plethora, the blood flow rate increases, new functioning capillaries open, the temperature of the hyperemic area is increased, redness of the hyperemic area is noted.
Arterial hyperemia most often manifests itself as a local pathological process that develops in a certain area, when more blood flows to it through the arteries than normal, and the outflow through the veins is normal. Usually it develops in connection with the expansion of small vessels (arterioles and capillaries) and contributes to the enhanced function of the organ, increasing its metabolism.
There are physiological and pathological arterial hyperemia.
1. Physiological arterial hyperemia is:
- working (functional) arterial hyperemia - an increase in blood flow in an organ due to the metabolic needs of a tissue or organ due to an increase in their functioning (arterial hyperemia of the skeletal muscles during exercise, an increase in coronary blood flow with increased heart work, a rush of blood to the brain during mental stress , increase in skin heat transfer with an increase in ambient temperature, etc.);
- postischemic (reactive) hyperemia - an increase in blood flow after its short-term restriction. Postischemic arterial hyperemia is observed after a temporary cessation of blood flow (temporary ischemia) and is of a protective and adaptive nature. Due to reactive hyperemia, the so-called blood flow debt is eliminated, a large amount of oxygen and nutrients are brought into the tissue, and metabolic products accumulated during ischemia are better removed.
2. Pathological arterial hyperemia develops under the influence of pathological stimuli (for example, with chronic inflammation, burns, fever, hypertensive crisis, allergies, etc.).
In most cases, arterial hyperemia is accompanied by an increase in metabolism and organ function, which is an adaptive reaction.
Arterial hyperemia in the absence of a need to increase blood flow and an excessive degree of hyperemia can also have a negative value.
Negative value of arterial hyperemia:
A sharp expansion of the vessel in atherosclerosis may be accompanied by a rupture of its wall and hemorrhage into the tissue, which causes the development of tissue edema. These phenomena are especially dangerous in the brain.
With injuries, increased arterial hyperemia plays a negative role.
After surgical interventions, arterial hyperemia also plays a negative role.
Venous congestionVenous hyperemia is an increase in the blood filling of an organ as a result of a decrease in the outflow of blood through the veins while slowing down the blood flow. This process is also called passive hyperemia or venous congestion.
With venous hyperemia, vein expansion is observed, they acquire a tortuous shape, blood flow through the veins slows down, the temperature of the hyperemic area is lowered, it acquires a bluish tint.
Reasons for the development of venous hyperemia:
- compression of the veins from the outside by a tumor, scar, adhesion, inflammatory edema, hypertrophied muscle, etc.;
- blockage of the veins from the inside by a thrombus;
- insufficient development of the elastic tissue of the veins or their valvular apparatus.
Venous hyperemia can be general and local. General venous hyperemia occurs due to decompensation of the activity of the cardiovascular system.
StasisStasis is a complete local cessation of blood flow in the vessels due to a primary violation of the viscosity (fluidity) of the blood.
With stasis, the inflow and outflow of blood in a static section of the microcirculatory bed are equal to zero, the capillaries can be expanded or narrowed.
The danger of stasis lies in its thrombogenicity. With true stasis, early and deep violations of the rheological properties of the blood occur.
Stasis is regarded as a manifestation of the failure of compensatory-adaptive mechanisms in the microcirculation system.
However, stasis can also play a positive role, for example, in inflammation, stasis prevents the spread and systemic action of agents that caused tissue damage, participating in the barrier function of inflammation.
IschemiaIschemia is a decrease in the blood supply to an organ or tissue due to a decrease in blood flow to its vascular network. This is the most important pathological process, one of the most common causes of hypoxia.
There are the following types of ischemia:
- obstructive - is the result of partial narrowing or complete closure of the lumen of the artery by a thrombus or embolus;
- compression - develops when the artery is compressed by a tumor, scar, etc .;
- angiospastic - occurs due to neurogenic spasm of the arteries (angiospasm).
Angiospasm is a pathological narrowing of the lumen of the arteries with a sharp restriction or even cessation of blood flow in them, resulting from excessive contractions of the vascular muscles for these hemodynamic conditions.
The nature of changes in the ischemic area is determined by the degree of oxygen starvation, the severity of which depends on the rate of development and type of ischemia, its duration, localization, the nature of the collateral blood supply, and the functional state of the organ or tissue.
Ischemia is a harmful process for the body, its outcome depends on the collateral circulation. Collaterals normally do not function and open in case of blockage of the main vessel.
The concept of infarction and necrosisA heart attack is a focal necrosis of an organ, which is the result of a sudden violation of local blood circulation (due to the cessation of arterial blood flow). A heart attack is a focus of necrosis with an outcome in the connective tissue.
Necrosis is the necrosis, death of a part of a tissue or organ of a living organism, accompanied by the irreversible cessation of their vital activity. Necrosis is always the result of cell damage.
ThrombosisThrombosis is intravital blood clotting in the lumen of a vessel.
A thrombus is a compacted mass of clotted blood or lymph, formed in vivo in the blood or lymphatic channel.
Platelets are the formed elements of the blood. These are small platelets. Platelets play a leading role in blood clotting.
The blood coagulation system (hemocoagulation system) keeps the circulating blood in a liquid state and prevents its loss through damaged vessels through the formation of blood clots.
Causes of intravascular thrombosis:
- damage to the vascular wall;
- changes in the composition of the blood;
- blood flow disorder.
Thrombosis is a physiological process, a protective component of tissue response to injury, which allows minimizing the consequences of bleeding, strengthening the walls of aneurysms, which is involved in contraction and healing of wounds.
However, if the thrombus is excessive, insufficient, or has lost its necessarily local, limited character, it can become a source of severe pathology. Thrombosis is included in the dynamics of other pathological processes and, above all, local circulatory disorders, inflammation.
EmbolismEmbolism is a typical pathological process caused by the circulation of particles (emboli) in the blood that are not characteristic of normal blood flow. Embolism is an important factor in barrier impairment in the development of a local tissue response to injury.
Thromboembolism is an embolism of a vessel by detached parts of a blood clot.
Tumor embolism is not just the result of detachment of malignant cells from the surface of the tumor. It is a complex process that provides tumor metastasis.
The tasks of "ordinary" medicine, which deals with the prevention and treatment of various diseases, that is, pathology, and modern sports medicine are opposite. The latter is aimed mainly at young, healthy people and is designed to expand their physiological potential - speed, strength, endurance, energy and ability to quickly recover. And although physical activity, often at the limit of possibilities, does not go unnoticed for the body, many at the same time are ready to put their own health at stake for the triumph of victory and a place on the podium. Photo above FOTOBANK.COM/GETTY IMAGES
When talking about sports medicine, we must first remember the most important moments in the history of sports in order to understand how far it has come since ancient times. It is known, for example, that diseases of the heart, lungs, spinal curvature, bone fractures and dislocations were treated long before the ancient era in Chinese medical gymnastic schools. The technique, which can be safely called "philosophical and gymnastic", is described in the book "Kung Fu" more than 600 years BC. e., and Chinese doctors use it to this day, along with other classical oriental methods of treatment.
IN Ancient Greece And Ancient Rome, where physical culture was an important matter in the education of young people, and preparation for sports competitions was an everyday life, the activity of a sports doctor did not stand out from general medical practice, although the use of, for example, physiotherapy exercises was known even before Hippocrates. In ancient India, elements of physical culture were an integral part of religious and philosophical ideas. To this day, hatha yoga is very popular - one of the oldest systems of physical culture, based on the implementation static exercises or postures - asanas. Muscle strengthening or relaxation in yoga is combined with a variety of psychological settings for concentration. It is worth seeing how athletes today, for example, athletes, are preparing to perform this or that exercise, how deeply they plunge into a kind of trance, how they achieve internal mobilization of forces, in fact, using ancient or similar methods. For example, Yelena Isinbayeva, world record holder in pole vault, always “whispers” something to her pole, as if reading mantras. Watching such actions, it becomes clear that the essence of all processes is the same: the concentration of will leads to the mobilization of all the resources of the body. Drawing a similar analogy, it is easy to come to the conclusion that the extreme states that a modern athlete, a Shaolin monk, and a yogi put themselves into are very close in essence. But the question is, what does the human body pay for those seconds of concentration when it can overcome the visible barriers of its physical capabilities?
Provocation and rehabilitationIn 1928, at the Olympic Games in St. Moritz, for the first time, the main difference between a sports doctor and other medical specialists was formulated. The fact is that the main task of big sport, the so-called sport of high achievements, is to artificially create a "superman". And this often causes serious damage to the body.
In other words, the essence of the work of a sports doctor is, firstly, in constant attention to the work of the musculoskeletal system, which is subjected to serious stress during a sports competition. Secondly, in an integrated approach to " sports work» organism: after all, diseases or injuries in sports can be caused by many factors - from physiological to psychological. Therefore, sports medicine should use the achievements of related areas and specialties: psychology, cardiology, pulmonology, orthopedic surgery, physiology, biomechanics and traumatology. This is an interdisciplinary field of medicine, designed not only to eliminate the consequences sports injuries but also to prepare the athlete's body for such conditions in order to exclude the very possibility of injury. The task is almost impossible, but, nevertheless, it is believed that the preventive activity of a sports doctor is almost more important than the clinical one.
The extreme loads that an athlete experiences, going, say, to set a world record, wear out his muscles and nervous system and make the athlete a “pensioner” by about 35 years old, and even earlier in some sports. This is where sports medicine is divided into two areas: “provoking” a person for a result and “rehabilitating”, which neutralizes the consequences. Moreover, rehabilitation can be very different: from physiological, eliminating the consequences of injuries, to psychological. (After all, a defeat or leaving a big sport for an athlete is an undoubted psychological trauma, about which hundreds of books have been written and many films have been shot.) So the fate of an athlete turns out to be paradoxical. With him, everything happens the same way as in the cinema and in general in any show business: first they build a beautiful scenery, then during the filming they blow it up, making spectacular shots, and then they begin to “sweep” ... The task is simple: do without human casualties. As sad as it sounds, this is not always possible.
How different is this medicine from non-sports medicine, which uses, for example, the same physiotherapy exercises or health-improving jogging solely to maintain a healthy state of the body, increase its efficiency, and without extreme impact on a person? Of course, such methods - let's call them general health - can also be used in sports, but only as secondary, supportive means. True, Hippocrates said that nature heals, and medicine is only a servant of nature, probably meaning that any effect on the body should activate its own hidden compensatory and regenerative forces. But in professional sports, such slogans have long been abandoned. Now, rather, the slogans sound like Michurin's: "We cannot expect favors from nature!"
In auto racing, especially such as the super-prestigious and technically “advanced” Formula 1 and the American Kart series, the cars have long ceased to look like themselves. The classic automobile scheme “frame - steering wheel - four wheels”, of course, remains in force, however, in fact, all the details separately are far from the car that we are used to seeing on the streets and highways. Appearance- not the most important thing. The question is that modern sport “squeezes dry” all the juices from metal, carbon fiber and other ultra-modern materials from which this very car is built. The loads designed to help achieve crazy speeds are such that until recently it was considered quite normal for an engine in racing mode to exist for just one race! But something else is important: the stress on the body of an athlete in a competitive mode is quite comparable to engine wear. It turns out that an athlete should also be enough for only one race? .. But replacing the parts of a car and the “components” of a person are not the same thing.
sports injuriesValery Kharlamov
The legendary hockey player suffered, as they say, for his sportsmanship, which was compared with high art. During the 1972 Super Series, in which the USSR and the NHL teams met, for the overall victory, Canada needed to win the remaining three matches in Luzhniki, which seemed incredible at the time. The second coach of the NHL team, John Ferguson, in the sixth match of the series, called the main fighter Bobby Clark to him, pointed to Kharlamov and said: “This guy should be touched with a club on the ankle.” Having received the installation, Clark broke Kharlamov's leg with a club blow. Ferguson later admitted: “We just realized that if he continues to play, then nothing will shine for us ...” For Valery, the Super Series-72 was completed, and for the USSR team it was lost. The hockey player was treated at CITO for a long time and, through the efforts of Zoya Mironova, managed to continue his career until 1981.
Irina Rodnina
In 1972, figure skaters Irina Rodnina and Alexei Ulanov became Olympic champions in Sapporo. However, soon the relationship between the partners went wrong, Ulanov decided to draw up a new sports couple with my future wife- figure skater Lyudmila Smirnova. Literally immediately after the psychological trauma, Rodnina had to endure the physical one as well. At one of the training sessions, Ulanov dropped her from support, the athlete hit her head on the ice and received a serious injury - a brain contusion. However, despite the categorical prohibition of doctors, Rodnina still won her last championship with Ulanov, and then continued her stellar career in tandem with Alexander Zaitsev. According to Rodnina, she lives without two vertebral discs, with a torn shoulder and Achilles, and even that same brain contusion reminds of itself with severe pain.
Nikolay Tishchenko
In the semi-finals of the football tournament of the 1956 Olympic Games in Melbourne against the Bulgarian national team, the defender of the USSR national team Nikolai Tishchenko fell unsuccessfully and broke his collarbone. Substitutions at that time were not allowed by the Olympic rules. Tishchenko was frozen at the fracture site, his arm was tightly bandaged to his torso, and he remained on the field. In itself, this fact was already an example of sports courage, but everything turned out even more surprising: a few minutes before the end of the match, the injured defender took part in a combination that ended in a goal by Boris Tatushin. So Tishchenko became the main character of the semi-finals. However, the injustice was that, due to a fracture, he could not play in the final, which the USSR team won. And according to the then existing situation, only those who entered the field in the decisive match were awarded gold medals.
Alexander Karelin
Three-time Olympic champion in Greco-Roman wrestling famous not only for three Olympic gold medals. There are also such facts in his career: in 1988 he became the champion of the USSR for the first time, although the day before he received a concussion. And at the 1996 European Championships, he received a severe injury - a separation of the pectoralis major muscle. For a wrestler, this actually means the end of participation in competitions, if not the end of a career. The Americans rubbed their hands: after the operation, our heavyweight will definitely lose to their favorite Matt Ghaffari. Karelin, however, managed to win gold medal, which is a unique achievement in the history of this sport.
Sergey Perkhun
Tragedies also happen in sports when injuries are incompatible with life. On August 28, 2001, in the Russian Football Championship, CSKA played with the Anji club from Makhachkala. In one of the episodes, CSKA goalkeeper Sergei Perkhun and Anji forward Budun Budunov collided heads in a jump. Both players were seriously injured, and Perkhun was taken off the field in an unconscious state, and further on the way to the hospital, he fell into a coma, resulting in clinical death. Doctors' conclusion: stop of cerebral blood flow followed by death of brain cells.
In professional sports, the tasks are quite clear: medals, prizes, achievements. Since all this also affects direct financial interests, cleanliness in sports has decreased lately. One of the main problems of modern sport is doping. It has already been written about in the pages of the magazine, but it is impossible to ignore this problem when talking about sports medicine. Here is what the head of the anti-doping inspection of the Russian Olympic Committee Nikolai Durmanov said about this:
In fact, we should not catch athletes with the help of sophisticated medical equipment, but first of all, offer them alternative medical programs. Because where there is no normal sports medicine, there will definitely be doping. He will occupy this niche with one hundred percent probability, because in general, without medicine, elite sports are basically impossible. Moreover, he is very dangerous without it.
Of course, for our compatriots, this problem has not yet become a national one, as in America, where it is especially relevant in the so-called street sports, which are catching up with traditional sports in terms of the number of people involved. But in the US, completely independent organizations are fighting doping. And in Italy and France, the fight against him was left to the power structures: carabinieri and soldiers with machine guns at the ready.
It is said that before the Sydney Games, the Chinese removed 25 of their top athletes from the plane. Apparently, and before Athens, they found it necessary to maintain a reputation. After all, the Olympics for China are not just Games. This is a feature of the portrait of a superpower, which they are so eager for. As for the nature of their victories, if doping plays any role in this, it seems to be the smallest. How else can a country with 14 million professional athletes perform? Hundreds of bases organized by the most in the best way, excellent sports specialists who know everything from traditional medicine to modern genetic engineering.
Sports medicine as a systemIn Russia, sports medicine has received state support since the 1920s, after N.A. Semashko put forward the slogan: "Without medical supervision there is no Soviet physical culture.” And although later we were talking more and more about physiotherapy exercises, in reality everything turned out to be much more serious. Along with many areas of life in the country, a “detachment” began to form, whose best friend was Comrade Stalin. In 1923, the first department of medical control was opened at the State Institute of Physical Education in Moscow (later renamed the Department of Physiotherapy and Medical Control). And in 1930, the Presidium of the Central Executive Committee of the USSR adopted a resolution according to which the leadership of medical control was entrusted to the health authorities. This became the fundamental basis of the state system of medical support for sports. The Central Research Institute of Physical Education was opened, and in it - a laboratory of medical control. Then, on the basis of the Central Clinical Hospital of the Ministry of Railways, the first Healthy Person Clinic was opened, where the characteristics of diseases in athletes were studied. In 1951, the USSR Ministry of Health began organizing medical and physical education dispensaries (VFD) in all republics, regions, large cities and regions of the country. It was they who laid the foundation for a fundamentally new system of medical support for sports, under which there was not only treatment and observation, but also a strict selection of the future “generation of winners”. Everything was part of the system for the country's sports to enter a serious international level. This required extensive scientific research on the medical problems of sports, and research needed "material" - millions of athletes, no matter how strange it sounded in a country depleted by war. In 1963, the Federation of Sports Medicine of the USSR appeared. So she became an independent direction. Now in Russia there is a huge network of medical and physical education clinics, dispensaries, where doctors are engaged in various areas of sports medicine. Of course, the commercialization that broke into our society in the late 1980s and early 1990s also affected their work, but the main state medical and scientific centers retained both specialists and the base of activity. Sports medicine is formally considered a clinical branch of biomedical science. However, in fact, as we have already noted, it is a completely independent branch of knowledge.
"Spare parts" and "mechanics"And yet, traditional sports medicine today is primarily concerned with the same "sweeping" - the treatment of injured athletes.
Not so long ago, a study was conducted on the health status of the winners and prize-winners of the largest international competitions. So: 98 champions out of 100 won with severe injuries behind them. For example, the Olympic champion gymnast Sergei Kharkov has become, as they say, a clear example of almost all the unique capabilities of CITO (Central Institute of Traumatology and Orthopedics named after N.N. Priorov). At first, a 20-cm metal plate was implanted in his lower leg, because the bone exfoliated from the exorbitant loads of the gymnast. Then there was a rupture and necrosis of the biceps - a piece of lavsan had to be sewn into the tendon so that the arm gained mobility. At the next competitions, Sergey's pectoralis major muscle came off, which was “reassembled” again. Then - a severe dislocation of the foot. It was adjusted with special needles and oxygen was supplied to the joint. This was followed by a rupture of the Achilles tendon ... Nevertheless, after the treatment, the champion continued to perform and win! The only question is what exactly the “broken” athlete will feel in old age. And the famous gymnast Elena Mukhina could not be returned to a full life after terrible injury- fracture of the spine. For a long time she remained disabled and died at the age of 46. Just as they failed to prevent the death of a 19-year-old football player in May this year Moscow region club"Saturn" by Kirill Spassky. He died his, more precisely, non-violent death - his heart could not withstand the stress.
Director of the Moscow Center for Sports Medicine, Honored Doctor of Russia Zurab Ordzhonikidze says that “overloads make the bones of an athlete, although hard, extremely fragile. Muscles and tendons change significantly, often when injured, they simply shatter into pieces, like children's balloons. That is why the treatment of sports injuries requires a special approach using certain technologies. Sports medicine is constantly updated with new means and methods of treatment. For example arthroscopy
, which replaced the usual joint surgery. Or shock wave therapy, when the damaged area of the body is affected by acoustic waves of a certain energy and frequency. Or endoprosthesis replacement - replacement of a worn or hopelessly damaged joint with an artificial one, which relieves constant pain, allows you to walk normally and lead a full life. And this is not only about the hip and knee joints but also shoulder, elbow and ankle. And in the surgical treatment of severe bone fractures and osteosynthesis, “spare parts” are used - modern lightweight and durable metal structures. It is clear why the achievements of sports medicine are also used in other areas of extreme medicine: military, space, disaster medicine.There are many scientific and clinical centers of sports medicine in the world. In Russia, this is primarily CITO, within which the Center for Sports and Ballet Trauma and Rehabilitation operates. Every year CITO performs 600-700 surgeries, treating up to 1500 patients. Since 1998, the Institute has been headed by the head of the Department of Sports and Ballet Injuries, Doctor of Medical Sciences, Professor Anatoly Orletsky. An internationally recognized specialist in sports and ballet injuries, he is also a consultant to the Russian Olympic Committee.
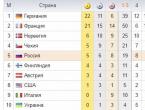
There are other well-known centers: the National Academy of Sports Medicine in the United States, the Sports Injury Clinic in the UK, the Canadian Academy of Sports Medicine, the Sports Traumatology Research Center in Norway, and the National Sports Medical Centers in China.
However, there are few good sports specialists, for example, in Russia. After all, the problems that the state system of domestic education is now experiencing have also affected sports medicine. Many state that at present, none of the educational institutions in the country trains personnel capable of really solving the issues of ensuring the medical and biological training of athletes. There are no training programs for doctors in the specialty "sports medicine" that meet modern requirements. And there are few professionals capable of creating curricula. Modern sports medicine has practically turned into the current work of doctors serving teams, for whom the main thing is tactical work. That is, the athlete's readiness to start.
Today in Russia there are four departments responsible for the large-scale development of sports in the country. These are the newly created Ministry for Sports, Youth and Tourism, Rossport, the Russian Olympic Committee and the parliamentary body - the Commission of the Federation Council for Youth and Sports. Sports medicine, on the other hand, does not actually fall under their jurisdiction, remaining part of the Ministry of Health system. It turns out fragmentation, which can be overcome only by a systematic approach. Various solutions to the problem are proposed, but so far everything rests on another classic quote: "Our land is rich, there is only no order in it."
Chapter III Fundamentals of General Human PathologyGeneral pathology is the study of the most general patterns of pathological processes, their main features that underlie any disease, regardless of the cause that caused it, the individual characteristics of the organism, specific environmental conditions, research methods (clinical, morphological, functional), etc. P.
General pathology serves primarily to study the biological aspects of medical problems and the very essence of human disease. The main goal of both general pathology as a whole and its individual sections is the development of a coherent doctrine of the disease. First of all, practical medicine is in dire need of this: only based on such a teaching, it is possible to develop the scientific foundations for disease prevention, give a correct assessment of the first clinical manifestations of the disease, clearly imagine the essence of its various periods, including relapses, and, as a result, increase rationality and effectiveness of medical intervention.
General pathology in present stage development is divided into three sections. One of them includes information on such issues as the periodization of the disease, the causes of its occurrence (etiology), the mechanism of development (pathogenesis) and recovery, the significance of the constitution, heredity, reactivity, etc.
The study of pathology in the course of sports medicine is necessary for students of institutes and faculties of physical culture of universities, primarily because athletes and schoolchildren (especially young athletes) often have a variety of diseases and changes in the musculoskeletal system (MSA). In some cases, this is due to the fact that, with insufficient medical supervision, people who already have certain diseases or deviations in health begin to go in for physical education and sports; in others - deviations in the state of health occur already in the process of playing sports. The appearance of injuries and diseases in athletes (especially in young athletes) is facilitated by training without taking into account their health and functional state, age, gender and other factors.
In order to correctly decide whether to continue training or stop them immediately, whether to seek advice from a doctor or provide an athlete with any first aid, etc., it is important for a teacher (coach) to know the main manifestations of pathology, to understand the causes and mechanisms of disease development.
Without knowing the general patterns of the occurrence of pathological processes (general pathology), it is impossible to understand the changes that occur in the body of athletes with certain diseases (private pathology). Acquaintance with private pathology is also necessary when studying the use of physical culture for therapeutic purposes in the rehabilitation system for various injuries and diseases, etc.
Knowledge of what health is, what disease is and under what conditions it occurs is an essential factor in the prevention of diseases and injuries in physical education and sports.
Health is such a state of the body in which it is biologically complete, able-bodied, the functions of all its components and systems are balanced, and there are no painful manifestations. The main sign of health is the level of adaptation of the body to environmental conditions, physical and psycho-emotional stress.
High adaptability of the body to changes in the external environment (temperature, humidity, hypoxia, etc.) is necessary for athletes during training and participating in competitions.
It should be noted that there is no boundary between the norm and pathology. There are various transitional stages between health and disease. The disease usually occurs when the body is subjected to excessive physical and psycho-emotional stress or when adaptive functions are reduced. Then morphological and functional changes occur, often turning into a disease or leading to an injury to the musculoskeletal system.
A disease is a process of transformation of a normal state into a pathological one, associated with reactive-determined changes in the degree of compensatory-adaptive self-regulation of living systems. The norm is a measure of the vital activity of the organism in given specific environmental conditions, within which changes in physiological processes are kept at the optimal level of functioning of homeostatic self-regulation. The disease is associated with the transformation of the normal state of a living system into a pathological one, that is, with the transition to a new qualitative state.
Any disease is a defeat of the whole organism. According to the nature of the course of the disease, they are divided into acute, subacute and chronic. Acute disease begins suddenly, immediately appear pronounced symptoms. Subacute disease proceeds more sluggishly. Chronic disease lasts for many months or years. Sometimes an acute illness becomes chronic. This is facilitated by insufficiently active treatment, and in sports - the early resumption of training or participation in competitions.
The concept of the disease includes the idea of the pathological process and the pathological condition.
A pathological process is a reaction of the body to a pathogenic irritation, which is based on a violation of the function of an organ or its structure. During the disease, various pathological processes can occur, for example, fever and inflammation of the glands with angina, fever and cough with pneumonia, etc.
A pathological condition is one of the stages of a pathological process or its consequence. An example of a pathological condition can be rheumatism, which later leads to heart disease, myocarditis, etc.
Identification and study of the causes of diseases are the basis of prevention. Most often, diseases occur as a result of external factors. However, diseases can also arise from internal causes that lie in the body itself. External (exogenous) causes - hypothermia, overheating, radiation, malnutrition, etc. - change the internal state of the body, resulting in reduced immunity, resistance to pathogenic factors. Internal (endogenous) causes of the disease are associated with heredity, constitution, reactivity, immunity, etc.
Pathogenesis is the study of the mechanisms of the onset, development and course of a disease. The pathological process can develop at various levels: molecular, tissue, organ, and finally, capture the whole system. It should be noted that in the body all cells, tissues and organs are inextricably linked. Therefore, there are no local diseases, the whole body is always sick. From this follows the basic principle of treatment: it is necessary to treat not the disease, but the patient (M.Ya. Mudrov).
During each disease, the following periods are distinguished: 1 - hidden, or latent; 2 - prodromal, or the period of precursors of the disease; 3 - the period of the developed course of the disease; 4 - the period of completion of the disease.
The latent (latent) period is the time from the introduction of a pathogen into the body until the first manifestations of the disease. In infectious diseases, the latent period is called the incubation period.
The prodromal period is manifested in malaise, headache, chills, fever, etc.
The period of the developed course for each disease has certain manifestations, is characterized by a combination of certain symptoms. The set of symptoms is called a symptom complex or syndrome.
The period of completion of the disease is different: recovery with restoration of functions, transition to a chronic form, complication or death.
With metabolic disorders in the body, various changes occur. It is known that all tissues require oxygen and nutrients with the timely removal of metabolites. The process of assimilation of nutrients is called assimilation, the process of decay is called dissimilation. Tissue nutrition is provided by the adaptive-trophic influence of the central nervous system.
Assimilation is a combination of the following processes of creating living matter: intake of substances necessary for the body from the external environment; the transformation of substances into compounds acceptable to body tissues; synthesis of cells, enzymes and other regulatory compounds and replacement of obsolete with new ones; synthesis of simple formations into more complex compounds; deposition of reserves.
Dissimilation - a set of the following processes of decay of living matter: mobilization of the body's reserves; splitting more complex compounds into simpler ones; decay of obsolete tissue and cellular elements; splitting of energy-rich compounds along with the release of energy; elimination of waste products from the body.
Other sections of the foundations of human pathology are dystrophy, circulatory disorders, inflammation, regeneration, etc.
Dystrophy is manifested in a violation of tissue (cellular) metabolism, leading to structural changes in tissues and cells. Therefore, dystrophy is considered as one of the types of damage. The immediate cause of the development of dystrophy can be violations of cellular or extracellular mechanisms. Among them are the following: disorders of cell autoregulation, leading to its energy deficit and disruption of enzymatic processes in the cell; disruption of the trophic transport systems, causing hypoxia, which becomes the leading one in the pathogenesis of dyscirculatory dystrophies; disorders of the endocrine or nervous regulation of trophism, underlying endocrine and nervous (cerebral) dystrophies.
Dystrophies are divided (depending on the predominance of morphological changes in the specialized elements of the parenchyma or in the stroma) into parenchymal, mesenchymal and mixed; (according to the predominance of violations of one or another type of metabolism) into protein, fat, carbohydrate and mineral; (depending on the influence of hereditary factors) on acquired and hereditary; (according to the prevalence of the process) into general and local.
It is known that various injuries and diseases of the nervous system cause various changes in tissues. Atrophy - a decrease in volume and a decrease in the functional activity of organs and tissues due to the death of cellular and tissue elements in any pathological process due to malnutrition of tissues or a long-term decrease in the degree of their involvement in the general physiological process.
Hypertrophy is an increase in an organ or part of it due to an increase in the volume and (or) number of cells. There may be vicarious hypertrophy (of one of the organs when the function of the other is turned off); hormonal (some organs); true (organ hypertrophy due to an increase in the size and number of its functioning parenchymal elements); compensatory (of an organ or part thereof, caused by an increase in activity that compensates for any disturbances in the body); corrective, when the function of another organ that is with it in a single functional system changes (usually some endocrine gland); false (organ hypertrophy due to the predominant or exclusive growth of its interstitial tissue or surrounding fiber); neurohumoral (as a result of violation of neurohumoral regulation of organ function); regenerative (true hypertrophy of a part of an organ that develops after resection or damage to another part of it); physiological (true hypertrophy due to an increase in the function of an organ in persons of physical labor, athletes, etc.).
Athletes who systematically train in cyclic sports may develop myocardial hypertrophy, that is, an increase in the heart muscle. Moreover: today it is believed that every athlete has myocardial hypertrophy in the initial stage. Hypertrophy of the myocardium, passing certain boundaries, contributes to the strengthening of the work of the heart, as was previously thought.
Various unfavorable factors play a decisive role in the development of myocardial hypertrophy in athletes: participation in competitions and training in a painful condition or after illnesses (SARS, influenza, tonsillitis, etc.), the presence of chronic foci of infections (dental caries, chronic tonsillitis, cholecystitis, furunculosis and etc.). The basis of pathological hypertrophy is the deterioration of the blood supply to the heart muscle, dystrophic changes that lead to a deterioration in myocardial contractility and, consequently, to a decrease in sports performance.
Quite often, when training in areas with a hot and humid climate, excessive passion for a bath (sauna), a violation of water and mineral metabolism occurs in the athlete's body. This manifests itself in changes in the acid-base state (ACH), electrolyte, water-salt and other indicators of homeostasis.
The acid-base state (ACS) ensures the normal functioning of the cell with a constant volume, composition and pH of body fluids. The acidity or alkalinity of solutions depends on the concentration of H4, an increase in it makes the solution acidic, a decrease - alkaline. The extracellular fluid is slightly alkaline, and its pH is in the range of 7.35-7.45.
Water-salt metabolism - a set of processes for the distribution of water and electrolytes between the extra- and intracellular space of the body, as well as between the body and the external environment. The distribution of water in the body is inextricably linked with electrolyte metabolism.
Water-electrolyte homeostasis - maintaining the constancy of osmotic volumetric and ionic balance outside and intracellular fluids of the body with the help of reflex mechanisms.
Water balance - the ratio between the amounts of water entering the body and removed from it.
Athletes, especially those who train in cyclic sports (runners-stayers, cross-country skiers, cyclists, etc.), have marching (spontaneous) bone fractures, convulsions, etc. Athletes who drive weight (wrestlers, boxers, weightlifters, etc.) with pharmacological agents and a bath often have serious violations of mineral (salt) metabolism.
Necrosis is the necrosis of a part of a living organism, the irreversible cessation of the vital activity of its elements. This is not just a local reaction of a cell, tissue or organ to damage, but a complete cessation of their vital activity (Scheme I).
Necrosis as a biological phenomenon cannot be considered only a pathological process, since it is a necessary moment in the development and functioning of the body. The cells of the epidermis of the skin, the epithelium of the mucous membrane of the gastrointestinal tract, and some glandular organs are constantly dying. Physiological autolysis is widespread in the body as a necessary part of the self-renewal of the system at the cellular, tissue and organ levels, but it has a different biological significance (organism development and morphological processes, tissue regeneration and growth, aging, physiological changes, etc.).
Necrosis as a pathological phenomenon can cause irreversible changes in the body up to death. Clinically, necrosis is expressed in specific diseases: myocardial infarction, limb gangrene, etc. In addition, necrosis can be an integral part, pathogenetic link of another process (inflammation, allergy) or disease (viral hepatitis, diphtheria, etc.).
The transition of an organ, tissue or cell from one qualitative state (life) to another (death) should be considered as a whole, cumulatively, and not by assessing and registering changes in a part.
There are two types of circulatory disorders: general, or central, affecting the level blood pressure, blood flow velocity, and local or peripheral, caused by resistance to blood flow in small vessels of individual organs and tissues, as well as blood filling of capillaries.
The determining factors of circulatory disorders are: damage to the heart, lungs, chest and diaphragms that affect the filling of the heart chambers; skeletal muscles and ligaments, disrupting the flow of blood to the heart through the veins; endocrine glands, affecting blood pressure and the exchange of electrolytes in the vascular wall; cortical and medulla of the kidneys, affecting through the system of renin and prostaglandins on blood pressure. Changes in the tone of arterioles and venules, which affect the resistance to blood flow, and changes in the rheological properties of blood, its viscosity, due to violations of the blood coagulation system or the properties of its formed elements, their relationship with plasma, also have a great influence on blood circulation.
Various periods of life and death of an organism and its elements
In morphofunctional terms, the vessels of distribution, resistance, metabolism, shunting and capacitance are distinguished. Regulation of blood circulation in vascular system carried out by both nervous and humoral mechanisms. In case of violation of the regulatory mechanisms of blood circulation, compensatory mechanisms are activated.
Compensation mechanisms in the vascular system depend on changes in the lumen of the vessels, blood deposition, collateral blood flow, venoarterial reaction (spasm of arterioles and small arteries in violation of outflow).
When analyzing the state of blood circulation in tissues, it is necessary to take into account the restructuring of the vessel walls and the width of the lumen in relation to vessels of all calibers, and not to individual vessels.
The pathological anatomy of circulatory disorders varies depending on the rate of development, the severity of the process, the angioarchitectonics of organs and the sensitivity of tissues to oxygen starvation.
Hyperemia - an increase in blood supply in any part of the peripheral system (small arteries, capillaries and veins), caused by an increase in blood flow to the microcirculatory system (arterial hyperemia) or a weakening of the outflow of blood (venous hyperemia). Arterial hyperemia can occur under normal conditions (as a manifestation of adequate regulation, i.e. corresponding to the metabolic need for blood supply to the tissue) and pathological (as a manifestation of compensatory regulation of blood circulation in certain disorders).
Types of arterial hyperemia: working (functional); postischemic (reactive, postocclusive, postcompression); collateral (around the focus of ischemia); inflammatory. Venous hyperemia is a pathological change in blood circulation that occurs when there is a violation of the outflow of venous blood.
Arterial plethora is more often active, acute;
in a healthy person, it quickly disappears, which is explained by the peculiarities of the reaction of blood vessels to stretching. Collateral arterial hyperemia proceeds for a longer time due to the disclosure of previously poorly functioning arteries or arterioles.
In a small circle, arterial hyperemia of shunting is possible, due to the presence of interatrial and especially interventricular defects during blood shunt from left to right. In this case, arterial blood enters the lungs along with the venous blood. Large branches of the pulmonary artery of the elastic and elasto-muscular type undergo expansion, and the vessels of the muscular type undergo narrowing. With the simultaneity of these processes, precapillary arterial hypertension of the small circle develops. Prolonged arterial hyperemia in any organ can cause vascular rupture, diapedetic bleeding, tissue edema.
Venous plethora is often called congestive or passive, as it occurs as a result of a violation of the outflow of blood through the veins due to a decrease in cardiac activity, compression or obstruction of the veins. Along with this, venous hyperemia is also active, in particular, in areas of collateral venous plethora (for example, in the mucous membrane of the esophagus, rectum, when opening co-portal anastomoses in conditions of liver cirrhosis).
Active nature is venous hyperemia during blood deposition. In humans, blood is deposited in the liver, spleen, subcutaneous tissue, etc. Prolonged venous hyperemia is accompanied by pronounced hypertrophy of the muscular layer of the veins. Depending on the architectonics of the veins in different organs, venous plethora manifests itself differently.
The consequences of venous hyperemia include varicose veins, hypoxic damage to tissues, blood cells, impaired lymph circulation.
Stasis is a non-specific phenomenon, it can also occur without previous venous plethora, under the influence of intoxication, as a result of the action of various physical and chemical agents on tissues. Distinguish between hemostasis and lymphostasis.
Hemostasis is a multicomponent system, the constituent elements of which are blood, vascular walls and organs that increase or decrease the ability to blood coagulation and the formation of vascular-active substances. This system helps to maintain the desired consistency of blood in the vessels and stop bleeding when they are damaged, and also affects the rheological properties of blood, microcirculation, vascular permeability, wound healing processes, and immunological reactions. Hemostasis is effective with close interaction of the coagulation, anticoagulation, fibrinolytic and kinin systems of the body.
Lymphostasis is called stagnation of lymph, which occurs as a result of mechanical, resorption or dynamic insufficiency of lymphatic movement. Mechanical insufficiency of lymph circulation is caused by an increase in venous pressure, as well as compression or blockage of the lymphatic vessels, spasms of the collectors, etc. Dynamic insufficiency is explained by a discrepancy between the excess of interstitial fluid and the rate of its removal.
Pastosity - diffuse swelling and a decrease in the elasticity of any part of the skin.
Bleeding is the process of escaping blood from blood vessels. Hemorrhage - a consequence of internal bleeding - accumulation of blood in tissues, cavities. According to morphology, three types of hemorrhages are distinguished: hematoma - hemorrhage with the formation of a cavity; hemorrhagic infiltration - impregnation of tissue with blood; petechiae and ecchymosis - pinpoint hemorrhages.
There are three causes of bleeding: rupture; corrosion of the walls of the vessel and non-damage of the wall - by diapedesis. The rupture of the vessel is often accompanied by the development of a hematoma, that is, a cavity containing liquid or clotted blood.
Bleeding by diapedesis, as a rule, arises from venules and capillaries. The reason is a violation of tone and permeability, which most often occurs as a result of hypoxia, intoxication, and also due to beriberi, blood clotting disorders, which underlie the so-called hemorrhagic diathesis, that is, a tendency to bleed. Diapedetic bleeding underlies the development of petechiae, ecchymosis, and apoplexy.
Ischemia - a decrease in blood flow to an organ - occurs when there is a significant increase in resistance to blood flow in the arteries that bring blood to this area, and there is no or insufficient collateral blood flow. Circulatory ischemia is called tissue anemia caused by a decrease or lack of blood flow to it, which may be due to angiospasm, arterial obstruction, thrombus, embolism, atherosclerotic plaque, sclerosis of the inner lining of vessels of various origins, etc. In the zone of anemia, there is a sharp slowdown in the metabolic process, which affects the immune system.
Heart attack - necrosis of a part (rarely - of the whole) of an organ, due to a violation of the blood supply. There is a heart attack, lungs, spleen, kidneys, etc. The most common myocardial infarction occurs when the coronary artery is obstructed in conditions of insufficient collateral function, as well as when the increased functional load does not correspond to the level of blood supply to the organ. Cardiovascular insufficiency (myocardial infarction) often occurs with intense physical exertion, overload, especially when training in the middle mountains.
Thrombosis is a pathological manifestation of hemostasis, that is, intravital blood coagulation with the formation of a clot in the lumen of the vessel, called a thrombus. It can completely or partially close the lumen of the vessel and cause serious circulatory disorders.
Embolism is a pathological process, which is characterized by the circulation in the vessels of the small and large circulation of foreign bodies that do not mix with blood, and blockage of blood vessels by them. These can be pieces of a detached blood clot, air or gas bubbles, droplets of fat, pieces of tissue, in particular, tumors, etc.
Inflammation is a complex local reaction of the body to tissue damage by various pathogenic stimuli. Inflammation is the result of the body's interaction with various pathogenic factors of the external and internal environment. External factors, or aggressive stimuli that can cause inflammation, include microorganisms, animal organisms, toxic and chemical substances, mechanical and thermal stimuli, medicinal substances, ionizing radiation, etc. Internal (autogenic) stimuli that cause inflammation include products of nitrogenous metabolism, decay of tumors (inflammatory reaction of the stroma), effector cells, mediators and immune complexes precipitating in tissues.
Inflammation is a multiphase process (alteration, exudation, proliferation), the development of which, in addition to pathogenic factors, is greatly influenced by mediators. Inflammation consists of interrelated and sequentially developing phases: 1) damage or alteration of tissues and cells (initial processes); 2) the release of mediators (triggers) and the reaction of the microcirculatory bed with a violation of the rheological properties of the blood; 3) manifestation of increased vascular permeability (exudation and emigration); proliferation.
The first phase - damage or alteration (dystrophy, necrosis) of tissues and cells (initial processes) with the release of mediators (triggers) - is biochemical. The second phase is the reaction of the microvasculature with a violation of the rheological properties of the blood, manifestations of increased vascular permeability in the form of plasmatic exudation and cell emigration, phagocytosis, and exudate formation. The third phase is cell proliferation with tissue repair or scar formation.
Trophy - a set of metabolic processes that underlie cellular nutrition and ensure the preservation of the structure and function of tissues and organs, regulated by the nervous system. The trophic function of the body ensures the full flow of metabolic processes, tissue nutrition, the constant adaptation of tissue structures to the requirements of the function, and the physiological regeneration of tissues.
Regeneration is the renewal of structures that have been lost as a result of pathological processes. There are two types of regeneration: 1) physiological, that is, the restoration of structures that die off during the normal life of the body; 2) reparative - restoration of structures after damage. Regeneration provides a wide range of adaptive reactions of the body, being the structural basis of its normal life. The terms of tissue regeneration are different, they depend on the blood supply to the tissue, the age and activity of the person. Thus, muscle tissue regenerates from 7 days to 12 days, bone - from 2-3 weeks to 4-6 months, tendons - from 4 weeks to 6 weeks or more, etc. The coach needs to know the terms of tissue regeneration, since if they are not observed, the early resumption of training leads to repeated injuries, sometimes even more serious, and more often to their transition to a chronic form. Regeneration is a biological process and cannot be accelerated. To improve the course of the regeneration process, massage, oxygen therapy, physiotherapy, hydrotherapy, exercise therapy, hydrocolonotherapy, etc. are used.
The desire to speed up the regeneration process muscle tissue with the use of massage, thermal procedures often leads to the occurrence of ossifying myositis.
A tumor is an atypical organoid formation that arose from the original germ (regardless of the interests of the organism) through the proliferation of its own elements, for which reproduction is an end in itself. Biochemically, a tumor cell differs from a normal one in the nature and activity of enzyme systems. The tumor is characterized by unresponsiveness of growth, its infinity, as well as the lack of the ability to differentiate its cellular elements.
All tumors are divided into benign and malignant. Benign tumors are only viciously developed tissue. These are uterine fibroids, breast fibroadenoma, congenital angiomas, prostate adenoma, neurinoma, etc.
Malignant tumors appear as a result of a special qualitative change in cells, their malignancy. Malignant tumors are characterized by metastasis, that is, the transfer of tumor cells outside the primary tumor with the formation of a tumor node in the distance. Cancer is characterized by a lymphogenous pathway of metastasis to regional lymph nodes. Sarcomas are characterized by a hematogenous route of metastasis.
Many questions of the etiology and pathogenesis of tumors are already close to being clarified. Thus, a connection has been established between the occurrence of tumors and radiation, with chemical carcinogens, viruses, with a violation of the hormonal status, with hereditary factors, etc.
Allergy is an abnormal (increased) sensitivity of the body to the effects of certain environmental factors (chemicals, microbes and their metabolic products, food products, etc.), called allergens. Allergic diseases (bronchial asthma, hay fever, urticaria, allergic rhinitis, dermatitis, drug and food allergies) are widespread throughout the world and tend to increase.
The reason for this, first of all, is the widespread use of antibiotics and other drugs, as well as the emergence of a large number of synthetic materials, dyes, washing powders, many of which can cause an allergic reaction.
Allergens can be various compounds, from simple chemicals (bromine, iodine) to the most complex (proteins, polysaccharides), and combinations of both. Some of them enter the body from the outside (exogenous), others are formed in the body itself (endogenous or autoallergens). Exogenous allergens can be of non-infectious origin (household dust, animal hair, drugs, chemicals, plant pollen, animal and plant foods) and infectious (bacteria, viruses, fungi and their metabolic products). Getting into the body in various ways, exogenous allergens can cause damage to various organs and systems.
Exogenous allergens are divided into the following groups:
Biological allergens - microbes, viruses, fungi, helminths, serum and vaccine preparations.
medicinal allergens. Almost any drug can cause an allergic reaction. The intensity of allergic reactions depends on how often and in what quantities the drugs are used. It must be remembered that taking any medication without a doctor's prescription is extremely dangerous.
Household allergens: house dust, fungi, mold on the walls of damp rooms, dead organs of domestic insects (cockroaches, bed bugs, bed mites). This group also includes the so-called epidermal allergens - hair, wool, animal dander, etc.
In recent years, the number of allergic reactions to household chemicals has increased, especially to washing powders.
pollen allergens. Most often it is the pollen of wind-pollinated plants, which causes a runny nose, conjunctivitis, etc.
food allergens. In practice, they can be almost all food products / More often than others, milk, eggs, meat, tomatoes, citrus fruits, chocolate, strawberries, strawberries, crayfish cause allergies. When allergens enter the body through the gastrointestinal tract, a food allergy occurs. Its symptoms are vomiting, diarrhea, urticaria, fever, etc.
Overfeeding contributes to the development of food allergies in children. Food allergens often cause diathesis. An intolerance to certain foods is not always an allergic reaction. It may be due to a lack of certain enzymes in the digestive juices, which leads to indigestion of food and disorders similar to food allergies.
industrial allergens. In our time, the number of various substances has increased, in contact with which allergic reactions occur, mainly in the form of skin lesions - allergic occupational contact dermatitis.
In hairdressing and beauty parlors, allergens can be hair dyes, eyebrows and eyelashes, perfumes, etc.
Physical factors make up a special group of allergens: heat, cold, mechanical irritation. It is believed that in many cases, under the influence of these factors, certain substances are formed in the body, which become allergens.
The development of allergies is facilitated by impaired functions of the nervous and endocrine systems, as well as brain injuries, negative emotions, and decreased adrenal function.
Prevention of allergic diseases consists in observing measures that prevent repeated contact with substances that have a pronounced sensitizing effect, and measures that prevent a violation of the body's defense reactions.
Household dust must not be allowed to accumulate in apartments. One of the measures is the elimination of foci of infection in the body, which are sources of sensitization (dental disease, inflammation of the paranasal sinuses, cholecystitis and other inflammatory processes). Normalization of the function of the gastrointestinal tract also reduces the possibility of developing food allergies.
In life, athletes are allergic more than ordinary healthy people. Excessive physical activity contributes to a decrease in immunity, especially in mid-mountain conditions, zones with a tropical climate, etc.
Allergies are caused by uncontrolled intake of a large number of medications (vitamins, protein preparations, panangin, potassium orotate, riboxin, etc.). An allergy occurs when taking fortified chocolate, flower pollen, with intravenous administration of protein preparations, etc. With the introduction of amino acids, athletes sometimes experience bronchospasm, Quincke's edema, a positive Pasternatsky symptom, and muscle pain.
When applying ointments to a diseased area of \u200b\u200bthe skin or massage with ointments, contact urticaria sometimes occurs - a special variant of allergic dermatitis. It usually appears a few minutes after the massage with some ointments and is characterized by the appearance of an urtic rash, itching, and hyperemia. An allergic reaction sometimes appears in a massage therapist: sneezing, coughing, hyperemia and a rash on the hands (forearms).
Athletes often react to taking medications with urticaria, one of the varieties of which is acute Quincke's edema. It is characterized by the sudden development of limited swelling of the skin (mucosa) and subcutaneous fat (lips, cheeks, eyelids, etc.). With edema developing in the larynx, asphyxia is possible, with the localization of edema in the eye sockets, there may be a deviation of the eyeball in the medial direction, a decrease in visual acuity.
Allergic rhinitis (rhinitis) is characterized by paroxysmal nasal congestion with copious watery-mucous discharge, sneezing.
If an allergic reaction occurs, the athlete is given plenty of fluids, sometimes an enema or laxative is indicated. They give antihistamines: tavegil, suprastin, diphenhydramine, pi-polfen, etc. Locally, anti-allergic drugs (ointments) are used for dermatitis, eye drops for conjunctivitis, cold for itching and scratching.
To prevent possible reactions, the body is hardened, vegetative-vascular dystonia is treated, etc. It is important to observe a healthy lifestyle, the correct mode of work and rest.
Immunity - immunity or resistance of the body to the action of pathogenic microorganisms and their toxins. It should be considered as a biological defense mechanism that allows the body to maintain a normal internal state (homeostasis), protecting it from exposure to infectious agents or any substances that have the properties of antibodies.
In addition to phagocytic cells, chemical compounds also take part in the immune reaction - antibodies, which are soluble protein substances - immunoglobulins (IgA, IgM, IgG, IgE), produced in response to the appearance of foreign proteins in the body. In plasma, antibodies stick together foreign proteins or break them down. Antibodies that neutralize microbial poisons (toxins) are called antitoxins. All antibodies are specific: they are active only against certain microbes or their toxins. If the human body has enough specific antibodies, it becomes immune to certain infectious diseases.
Distinguish between innate and acquired immunity. Innate immunity provides the body with immunity to a particular infectious disease from the moment of birth. Immune bodies can cross the placenta from the vessels of the mother's body into the vessels of the embryo, or newborns receive them with mother's milk. Such passively acquired immunity ensures that newborns are immune to certain infectious diseases.
Acquired immunity appears after the transfer of any infectious disease, when specific antibodies are formed in the blood plasma in response to the ingress of foreign proteins into the body. In this case, there is a natural, acquired immunity.
Immunity can be developed artificially if weakened or killed pathogens of any disease (for example, diphtheria, scarlet fever, smallpox, etc.) are introduced into the human body. Against weakened microorganisms, antibodies are produced that neutralize the waste products of living organisms. Such immunity usually lasts for years. Immunity acquired by introducing immune serum from the blood of animals or humans into the body is called passive.
In addition to acquired immunity, so-called non-specific protective factors play an important role in protecting the body from pathogens of infectious diseases. These include the impermeability of healthy skin and mucous membranes for most microorganisms, the presence in skin secrets and in the enzymes of the stomach of substances that adversely affect microorganisms, the presence in the blood and body fluids (saliva, tears, etc.) of enzyme systems that irritate microorganisms (for example, lysozyme, properdin, etc.).
It has also been established that viruses, toxins and decay products of microorganisms are excreted from the body with sweat, sputum, urine, and feces.
Nonspecific protection factors also include an increase in the patient's body temperature, which contributes to recovery, for example, in viral diseases (influenza, SARS), since the reproduction of some viruses is delayed at temperatures above 37 ° C.
It is known that psycho-emotional overloads (disorders) in athletes during the period of preparation for responsible starts (competitions) reduce the body's resistance to infections. Negatively affects the immune system and leads to a violation of the production of immunoglobulins, insufficient intake of animal proteins, microelements.
With intense physical exertion, a number of athletes have a breakdown of adaptive mechanisms. Hypoxemia and tissue hypoxia are also associated with the functioning of the immune system in high-class athletes. A decrease in immunoglobulins leads to an increase in the level of infectious (colds) diseases and an increase in the number of injuries and diseases of the musculoskeletal system.
Thermoregulation - maintaining body temperature within a limited range when the level of internal heat generation and ambient temperature changes - is provided by means of autonomous thermoregulation.
Autonomous thermoregulation - a reaction to a decrease or increase in the temperature of the internal and external environment, consists in managing the processes of heat production and heat transfer (changes in peripheral vasomotor tone, sweating, thermal tachypnea, cold shivering). Autonomous thermoregulatory reactions can be carried out without the participation of consciousness.
The thermal balance of the body is a stationary state of heat exchange between the body and the environment, in which the heat content does not change.
Heat stroke is a painful condition caused by overheating of the body. It is expressed by headache, nausea, vomiting, fainting. The main reason for overheating of the body is a violation of thermoregulation that occurs during prolonged exposure to high ambient temperatures, especially in humid air, when sweating is ineffective. With heat stroke, body temperature can reach 40-41 ° C.
Heat transfer in physiology is the exchange of thermal energy between the body and the environment. It is carried out by conduction (conductive heat transfer), convection (convective heat transfer), radiation (radiative heat transfer) and evaporation (evaporative heat transfer).
Heat transfer in physiology is the process of dissipating heat into the environment through convection, radiation, evaporation, or a combination of them from a unit of body surface area per unit of time (W m-2).
Heat production in physiology is the formation of heat in the body due to metabolic processes. Total heat production is equal to the amount of metabolic energy minus external work.
Violation of thermoregulation during training and especially at competitions in areas with a hot and humid climate is a fairly common occurrence.
Disorder of thermoregulation is also observed in many diseases.
Desynchronosis occurs during international competitions, in various climatic and time zones, which impose increased requirements on the functional state of an athlete. If they are not observed, then various undesirable changes may occur that worsen the performance and health of the athlete.
It is well known that during the day there are rhythmic fluctuations in the activity of the physiological systems of the body. It has been proven that during the day almost 50 physiological functions change in the human body. Due to their rhythm, long-term performance of individual organs and the body as a whole is maintained. The main daily cycle, base, background for the existence of all other rhythms is the alternation of sleep and wakefulness, which are inextricably linked.
When flying through several time zones, one can observe a mismatch of rhythms, which forces the athlete's organs and systems to rebuild their functions, adapting to the influence of external factors. But it takes time to adapt. The terms of acclimatization depend on the functional training (fitness) of the athlete, his age, etc. gender. Since modern sport creates extremely high physical and psycho-emotional stresses for athletes, a change in climatic and geographical zones (belts) often leads to desynchronosis, or dysrhythmia.
Desynchronosis - changes in the body due to violations of its circadian (circadian and daily) rhythms. The coherence of the circadian system of the body directly depends physiological state; violation of rhythms is expressed in various deviations from the norm.
The main causes of desynchronosis: 1) mismatch of time sensors and circadian rhythms of the body - a) change of time zones (transmeridian flights, movements over long distances in the latitudinal direction); b) stable mismatch of sleep-wakefulness with the local system of time sensors (alternation of day and night shifts); 2) the impact of various physical factors (heat-cold, radiation, etc.), mental (especially emotional) stress, muscle (physical) stress, etc.
Symptoms of desynchronosis are reduced to sleep disturbance, loss of appetite, mood, mental and physical performance, various neurotic disorders, etc. In some cases, there is an exacerbation of diseases.
Most people experience undulating changes in working capacity during the day with two “peaks”: the first is from 8 am to 1 pm, the second is between 4 pm and 7 pm. At other hours, the functional level of the body is significantly reduced. This is directly related to the planning of the training process and the rest of athletes. With two workouts per day, higher (intense) loads should be assigned to hours of increased working capacity (activity), and lower ones - to hours of reduced working capacity.
Each flight to a different time zone requires a restructuring of metabolic processes in the body. Since metabolic processes (rhythms) are genetically laid down, their "breaking" does not pass without a trace. A sharp change in the diet is harmful, the products also should not differ sharply from the usual, especially in the first 5-7 days.
An athlete's adaptation to the time zone depends on the difference in time, age, functional state and health of the athlete.
Release year: 2003
Genre: Therapeutic exercise
Format: PDF
Quality: Scanned pages
Description: The textbook "Sports Medicine" outlines the basics of general and particular pathology in the aspect of sports medicine, the principles of conducting staged, current and urgent medical and pedagogical control over representatives of various sports specializations, issues related to medical support for competitions, as well as pre-pathological and pathological conditions in athletes, including emergency. Special sections are devoted to the peculiarities of medical control over young athletes, female athletes and older people involved in health-improving forms of physical culture. The publication contains a brief glossary of medical terms necessary for better assimilation of the material.
The textbook "Sports Medicine" is intended for students and teachers of secondary and higher educational institutions of physical culture, as well as secondary and higher educational institutions of a medical profile.
Chapter 1. DOMESTIC SPORTS MEDICINE: HISTORY OF DEVELOPMENT, GOALS, OBJECTIVES AND PRINCIPLES
1.1. The history of the development of domestic sports medicine (N.D. Graevskaya)
1.2. Goals and objectives of domestic sports medicine
1.3. Principles of organization of national sports medicine
Chapter 2. BASES OF GENERAL PATHOLOGY
2.1. Concept of health and disease
2.2. The main forms of the onset, course and end of the disease. Outcomes of the disease
2.3. Terminal States
2.4. Etiology and pathogenesis
2.5. Clinical representations of the constitution
2.6. Pathological heredity
2.7. Body reactivity
2.8. Immunological reactivity
2.8.1. The concept of immunity
2.8.2. Natural resistance factors
2.8.3. The concept of immunodeficiency
2.8.4. Acquired Immunodeficiency Syndrome (AIDS)
2.8 5 Allergy
2.9. Typical pathological processes
2.9.1. Circulatory disorders
2.9.2. Metabolic disorders in tissues
2.9.3. Necrosis
2.9.4. Inflammation
2.9.5. Atrophy
2.9.6. Hypertrophy
2.9.7. Tumors
Chapter 3. CLINICAL AND PARACLINICAL EXAMINATION METHODS
3.1. Clinical Methods surveys
3.2. Paraclinical examination methods
3.2.1. Anthropometry (E.K. Ermolenko)
3.2.2. Body thermometry
3.2.3. Instrumental-functional examination methods
3.2.4. Radiation diagnostic methods
3.2.5. Ultrasound diagnostic methods
3.2 6. Radioisotope diagnostics
3.2.7. thermal imaging
3.2.8. Endoscopic research methods
3.2.9. Laboratory research methods
3.2.10. Functional testing
3.3. Nervous system Basic methods of examination. Separate syndromes in diseases of the nervous system
3 3 1. Neurological examination
3.3.2. Separate syndromes in diseases of the nervous system
3.4. The cardiovascular system. Basic methods of examination Separate syndromes in diseases of the cardiovascular system
3.4.1. Examination of the cardiovascular system
3.4.2. Separate syndromes in diseases of the cardiovascular system
3.5. System of external respiration. Basic methods of examination. Separate syndromes in diseases of the respiratory system
3.5.1. Examination of the external respiratory system
3.5.2. Separate syndromes in diseases of the respiratory system
3.6. The digestive system. Basic methods of examination. Separate syndromes in diseases of the digestive system
3.6.1. Examination of the digestive system
3.6.2. Separate syndromes in diseases of the digestive system
3.7. urinary system. Basic methods of examination. Separate syndromes in diseases of the urinary system
3.7.1. Examination of the urinary system
3.7.2. Separate syndromes in diseases of the urinary system
3.8. The blood system. Basic research methods. Separate syndromes in blood diseases
3.8.1. Examination of the blood system
3.8.2. Separate syndromes in diseases of the blood system
Chapter 4
4.1. Primary and annual in-depth medical examinations
4.1.1. Principles of organizing primary and annual in-depth medical examinations
4.1.2. Principles of health assessment in the practice of sports medicine
4.1.2.1. The main diseases and pathological conditions that are a contraindication to sports
4.1.2.2. Athlete Health Questionnaire (Injury and Medical Record System)
4.1.2.3 Principles for the admission to sports of persons with borderline conditions
4.1 3. Principles of examination of the musculoskeletal system in athletes (E.K. Ermolenko)
4.1.4. Somatotyping
4.2. Staged medical and pedagogical control over representatives of various sports specializations
4.2.1. Principles of organization of stage control
4.2.2. Principles of studying the functional capabilities of the central nervous system
4.2.3. Principles of studying the functional capabilities of the neuromuscular apparatus
4.2.4. Principles of studying the functionality of the vestibular analyzer
4.2.5. Principles of studying the functionality of the visual analyzer
4.2.6. Principles of studying the functionality of the cardiorespiratory system
4.2.7. Principles of studying the functional capabilities of the external respiration system
4.2.8. Principles of the study of general physical performance
4.2.9. Principles of studying the energy potential of the body.
4.3. Current and urgent medical and pedagogical control over representatives of various sports specializations
4.3.1. Principles of organization of current control
4.3.2. Principles of organization of urgent control
4.3.3. Indicators of the current and urgent functional state of the central nervous system
4.3.4. Indicators of the current and urgent functional state of the autonomic nervous system
4.3.5. Indicators of the current and urgent functional state of the neuromuscular apparatus
4.3.6. Indicators of the current and urgent functional state of the analyzers
4.3.7. Indicators of the current and urgent functional state of the cardiovascular system
4.3.8. Current changes in the morphological and biochemical composition of blood
4.3.9. Indicators of the urgent functional state of the body
4.4. Principles of self-control
Chapter 5. FEATURES OF MEDICAL AND PEDAGOGICAL CONTROL OF YOUNG ATHLETES
5.1. Pathological hereditary predisposition and high risk of latent pathology
5.1.1. Minor developmental anomalies in children and adolescents
5.1.1.1. Anomalies in the development of the spine (0.0. Lagoda)
5.1.1.2. Cryptorchidism in male children and adolescents
5.2. Diseases of the musculoskeletal system, typical for childhood and adolescence
5.3. Principles for assessing the level of physical development and puberty in children and adolescents
5.3.1. Assessment of the level of physical development
5.3.2. Somatotyping of children and adolescents
5.3.3. Principles for assessing the degree of puberty of children and adolescents
5.4. Principles for assessing the functional state of the cardiorespiratory system in children and adolescents
5.4.1. Methodology for conducting and principles for evaluating functional tests with physical activity in children and adolescents
5.5. Principles for assessing general physical performance in children and adolescents
5.6. Features of the organization of physical culture and sports in childhood and adolescence (together with O.O. Lagoda)
5.7. Terms of admission to physical culture and sports for children and adolescents and age stages of sports training
Chapter 6
Chapter 7
7.1. Medical and pedagogical control in the middle mountains
7.1.1. Stages of adaptation to barometric hypoxia
7.1.2. Pedagogical aspects of construction training process in mid-mountain conditions
7.1.3. Sports performance in the period of reacclimatization after training in the middle mountains
7.1.4. Medical support of the training process in mid-mountain conditions
7.1.5. Alpine diseases
7.2. Training and competition in conditions of high and low temperatures
7.2.1. Sports activities in high temperatures
7.2.2. Sports activities in low temperatures
7.3. Resynchronization of circadian rhythms of an athlete's body after long-distance flights
7.3.1. Flight to the west
7.3.2. Flight to the east
Chapter 8. MEDICAL SUPPORT FOR SPORTS COMPETITIONS
8.1. Principles of organizing medical support for sports competitions (L.N. Markov)
8.2. Features of medical support for martial arts competitions
Chapter 9. Principles of organization of anti-doping control
Chapter 10
10.1. A complex of medical examinations for admission to health-improving physical culture
10.2. Principles for determining the level of physical condition of persons involved in fste culture
10.2.1. Methods! express assessment of the level of physical condition
10.2.2. Principles for determining the level of general physical performance in middle-aged and elderly people
10.3. Motor modes in the system of health-improving physical culture
10.4. The number and content of physical exercises for the development and maintenance of physical condition
Chapter 11
11.1. Compensation for fluid and electrolyte deficiencies in sports activities
11.1.1. Rehydration directly in the process of long-term muscle activity
11.1.2. Post-exercise compensation of fluid deficiency in the body
11.2. Sleep optimization in athletes
11.3. Optimization of nutrition and elimination of factors that impede the maximum implementation of the detoxification function of the liver in conditions of intense muscle activity
11.4. The use of pharmacological agents in order to optimize the processes of post-exercise recovery and increase physical performance
Chapter 12
12.1. Overwork
12.2. Overtraining
12.2.1. Type I overtraining
12.2.2. Type II overtraining
12.3. Chronic physical stress
12.3.1. Chronic physical overexertion of the cardiovascular system
12.3.2. Chronic physical overexertion of the system of nonspecific protection and immunity
12.3.3. Recurrent acute manifestations of chronic physical overexertion
12.3.3.1. Overstressing the digestive system
12.3.3.2. Overstressing the urinary system
12.3.3.3. Overstrain of the blood system
Chapter 13
13.1. Chronic overexertion of the musculoskeletal system
13.2. Acute injuries of the musculoskeletal system in athletes
13.2.1. Injuries to muscles, tendons and auxiliary apparatus of the joints
13.2.2. bone fractures
13.3. Sports and pedagogical direction of prevention of injuries and diseases of the musculoskeletal system in athletes
13.3.1. Techniques for applying teip bandages to various parts of the body
13.3.2. Permissible terms for the resumption of training sessions after injuries of the musculoskeletal system
Chapter 14. DISEASES AND INJURIES IN ATHLETES
14.1. The structure of morbidity in athletes
14.2. Diseases most frequently encountered in the clinical practice of sports medicine
14.2.1. Central and peripheral nervous system
14.2.2. The cardiovascular system
14.2.3. Respiratory system
14.2.4. Digestive system
14.2.5. urinary system
14.2.6. Musculoskeletal system
14.2.7. ENT organs (nose, throat, ear)
14.2.8. Organ of vision
14.3. Diseases that can cause sudden death during physical education and sports
14.3.1. Heart disease
14.3.2. myocardial infarction
14.3.3. Cardiomyopathy
14.3.4. Acute disorders of cerebral circulation
14.4. Acute injuries in athletes
14.4.1. Closed craniocerebral injury
14.4.1.1. Brain concussion
14.4.1.2. Contusion (contusion) of the brain
14.4.1.3. Brain compression
14.4.1.4. Features of traumatic brain injury in boxers
14.4.1.5. Craniocerebral injuries during martial arts
14.4.2. Closed injuries of the spine and spinal cord
14.4.3. Injuries internal organs
14.4.4. Injuries to the nose, ear, larynx, teeth and eyes
Chapter 15. SUDDEN DEATH IN SPORTS
Chapter 16
16.1. Anaphylactic shock
16.2. Sudden cessation of circulation
16.3. hypoglycemic state. Hypoglycemic coma
16.4. myocardial infarction
16.5. chest compression
16.6. fainting
16.6.1. psychogenic syncope
16.61.2. Vasovagal syncope
16.6.3. orthostatic syncope
16.6.4. Gravity swoon (shock)
16.7. Acute physical stress
16.8. hypothermia
16.9. Thermal lesions
16.9.1. Heat (sun)stroke
16.9.2. thermal collapse
16.9.3. Heat cramps
16.9.4. Heat exhaustion
16.9.5. General dehydration
16.9.6. Thermal swelling of the legs and feet
16.10. Drowning
Chapter 17. ACCIDENTS AND EMERGENCIES IN SPORTS: LEGAL FRAMEWORK (A.L. Vlasov)
17.1. Leadership Responsibility
17.2. Responsibility of the coaching and teaching and instructor staff
17.3. The responsibility of those involved
17.4. The order of consideration and analysis of the causes of emergencies and accidents in sports
Concise Dictionary of Medical Terms
Literature
Physical culture and sports in any civilized society are an objective need and perform important social functions, including the functions of preventive medicine. Their healing effect is associated with the strengthening of the biological mechanism of the body's protective and adaptive reactions, with the training effect of physical activity. In modern society, replete with emotional stress against the background of progressive hypokinesia, improving the level of health and functional state of a person is impossible without the wide and comprehensive use of physical culture, which should become an integral, mandatory part of the lifestyle. Sports activities, i.e. performance of exercises of high volume and intensity, of a specific orientation, pursue the goal of not only improving health, but also achieving high results, increasing sportsmanship in a particular sport. And in this regard, it is very important that sports achievements grow as a result of improved health, and not at the expense of health. It is no coincidence that biomedical knowledge forms the basis of the professional training of a future teacher (trainer), without mastering which he will not be able to competently build the process of physical education. Professionally, both teachers (trainers) and doctors are very close to each other, since the object of their attention is a living person, and both of them must adhere to the principle (non nocere - do no harm) in their work.
SPORTS MEDICINE is a science that studies the positive and negative effects of various degrees of physical activity (from hypokinesia to hyperkinesia) on the body of a healthy and sick person in order to determine the optimal physical activity for: a) strengthening and restoring health, b) increasing the level of functional state, c) growth of sports achievements, d) prevention and treatment of various diseases (A.G. Dembo, 1980).
The main goal of sports medicine is to promote the rational use of means and methods of physical culture and sports for the harmonious development of a person, maintaining and strengthening his health, increasing efficiency and achieving high sports results, prolonging an active, creative period of life (V.L. Karpman, 1987).
The main goal and content of sports medicine determine the objectives of the sports medicine course studied by students of the Academy of Physical Culture:
1) deepening and expanding the general biological and general medical training of future teachers and trainers;
2) teaching available methods of monitoring the health and functional state of people involved in physical culture and sports, evaluating the data obtained and using them in building the training process;
3) training in the use of knowledge and skills in the field of medical control, exercise therapy, massage in future activities;
4) fostering the need to work in contact with a sports doctor and an attending physician.
Sports medicine in its current form was not formed immediately, but went through several stages in its development.
At present, sports medicine is an established independent branch of medicine with its own tasks, organization, material and scientific base. All medical institutes and academies of FC have departments of sports medicine. In the bowels of sports medicine, its sections were formed: sports cardiology, traumatology, endocrinology, pharmacology, immunology, children's sports medicine, etc. The scientific potential of sports medicine has significantly increased, represented today by the established schools and scientific directions of professors A.G. Dembo, V.L. Karpman, Z.S. Mironova, N.D. Graevskaya, R.D. Dibner, S. Khrusheva, etc.
I.2 Dispensary method of monitoring athletes and athletesMEDICAL CONTROL is the main section of sports medicine. The content and tasks of medical control:
- assessment of the state of health, the solution of the issue of admission and sports orientation, taking into account indications and contraindications;
- control over the state of health during classes or the training process;
- assessment of physical development and its dynamics;
– diagnostics of the functional state;
- identification of the influence on the body of the regimen and methods of training;
– treatment of sports injuries, diseases and injuries in people involved in sports and sports, studying the causes of their occurrence and developing preventive measures;
- control over the compliance of the conditions and organization of classes with the accepted sanitary and hygienic standards;
– medical support of competitions; sanitary-educational and educational work.
The main form of organization of medical control over persons involved in physical culture and sports is DISPENSERIZATION. The essence of the medical examination method is the systematic medical observation of the health of a certain category of people - healthy or sick. Clinical examination of healthy people is carried out in relation to children, pregnant women, certain groups of production workers, as well as athletes. Tuberculosis, oncological, skin-venereal, etc. have been created for a certain contingent of patients. dispensaries. The medical and physical dispensary (VFD) is a scientific and practical center that provides guidance and direct medical care to people involved in physical culture and sports. First of all, highly qualified athletes, members of the national teams of the city, district, region, country are attached to the dispensary. At the same time, the WFD is the organizing center for the physical education of children and adolescents, supervises the work of school doctors in this direction, doctors of children's and youth sports schools, and health groups. At the same time, the WFD is responsible for managing the entire medical physical culture on the scale of the territory served by the dispensary. As a medical institution, the WFD is under the jurisdiction and subordination of the health authorities. Medical and physical education dispensaries are medical and preventive institutions that include physicians - therapists who oversee certain sports, doctors of narrow specializations (surgeon, ophthalmologist, otorhinolaryngologist, dentist, gynecologist, etc.), offices and departments of functional diagnostics, physiotherapy, physiotherapy exercises, clinical and biochemical laboratory, X-ray room.
I.3 Medical examination, its goals and objectivesDuring a medical examination of people involved in physical culture and sports, the following tasks are consistently solved:
1) determination of the state of health,
2) determination and assessment of the level of physical development,
3) assessment of the functional state of the body.
TYPES OF MEDICAL EXAMINATION:
- Primary is held for everyone who wants to engage in physical culture or sports. At the same time, the issue of admission to classes is resolved, Recommendations are given on the sport, taking into account the age, morphological and functional characteristics of the person.
- Repeated, is the essence of dispensary observation - the determination of the influence (both positive and negative) of physical exercises on the body. With their irrational use, repeated examinations allow timely detection of prepathological and pathological changes that require timely treatment.
- Additional are carried out after breaks in training caused by illness, injury or any other reasons. Additional examinations include medical examinations carried out before competitions in some sports (for example, in boxing).
The main principles of medical examination are:
- The systematic nature of medical examinations involves conducting examinations according to the plan, systematically, at certain intervals, established by the doctor, regardless of the well-being of the athlete or athlete. Thus, persons subject to clinical examination are required to undergo a full medical examination at least once or twice a year.
- The complexity of the medical examination involves a comprehensive examination of the body using a wide range of medical examination methods.
- the functional orientation of medical examinations means the need to study the body not only at rest, when an idea of \u200b\u200bfunctional capabilities is compiled, but mainly under the influence of various dosed factors (functional tests). In this case, the functional abilities of the organs and systems of the body as a whole are determined, i.e. the ability to use their abilities.
I.4 Methods of medical examination, their classification CLASSIFICATION OF METHODS OF MEDICAL EXAMINATION:1) clinical,
2) instrumental,
3) laboratory,
4) functional tests.
CLINICAL METHODS include:
- Anamnesis (translated from Greek anamnesis - recollection) is the totality of information reported by the patient to the doctor and used in establishing the diagnosis and prognosis of the disease. Passport details, marital status, place of residence, living conditions, education, profession are the so-called general anamnesis. When collecting a medical history, they find out what diseases, injuries, surgical interventions the subject underwent, when it happened. Data on diseases in the family and among relatives are analyzed in order to determine hereditary predisposition. Bad habits (smoking, drinking alcohol) are being clarified. A significant part of the medical history is made up of complaints of sick patients or subjective feelings of objective ill-being in the body. A sports history is collected from people involved in physical culture and sports, includes information about the sport, the duration of classes, the sports category, the nature of the training loads used, their volume and intensity, the number of training sessions per week. Of particular interest to the doctor is information about the growth of sports achievements or their absence (since what time, what preceded this, the alleged reason), whether there were any workouts in a painful state, whether there were signs of overwork and overstrain (if there were, then when and which ones were taken measures to eliminate them). To a certain extent, both the teacher and the trainer should master the methodology of collecting an anamnesis, since the data obtained in this case are of considerable interest to them and should be used in planning and organizing the training process.
- Somatoscopy - an external examination of the body is one of the methods for determining physical development, which allows you to assess posture, the state of the musculoskeletal system, body type. During a medical examination, an external examination also allows you to determine the patient's facial expression, the color and condition of the skin and mucous membranes (for example, pallor, redness or yellowness of the skin, cyanosis - cyanosis - mucous lips), the degree of fatness (obesity, emaciation), the presence of varicose veins etc.
- Palpation - palpation. With the help of touch, the turgor (elasticity) of the skin, various painful points in the tissues, fluctuations in the walls of the arteries (rhythm, filling of the pulse, heart rate), the presence and degree of enlargement of the lymph glands, the state of the abdominal organs (the presence of seals, soreness), etc. .
- Percussion - percussion. This research method is based on the fact that the nature and intensity of the sound that occurs when a finger is tapped on a part of the body of the subject depends on what is under the place of tapping - a dense body, liquid or air. For example, when percussion of the chest over healthy lungs filled with air, a clear sound is heard, but with inflammation of the lungs, the presence of a tumor in them, percussion will dull the sound. The method allows you to identify foci of inflammation, the presence of fluid, tumors, determine the size and position of some organs.
- Auscultation listening. By using this method studies listen to sound vibrations that occur during the work of internal organs (for example, heart sounds and murmurs, respiratory noises and wheezing, heard in the lungs when air passes through the bronchial tree, etc.).
INSTRUMENTAL research methods used in medical and sports practice allow a deeper and more accurate assessment of the state of human organs or systems. So, in the study of the functional state of the circulatory system, devices for measuring blood pressure (sphygmomanometers), devices for studying the work of the heart (electrocardiographs, phonocardiographs, echocardiographs) are used. The study of the functional state of the external respiration system involves the use of spirometers and spirographs, pneumotachometers, pneumotonometers, oximeters, etc.
LABORATORY METHODS of research include:
– Biochemical studies of liquid media and body secretions
– Microscopic analyzes of liquid media and body secretions (blood, urine, gastric juice, bile, sputum, feces, etc.)
– Histological studies of tissues (study of cellular composition)
– Bacteriological methods (determination of the presence of bacteria, viruses, fungi, etc. in liquid media and body secretions)
FUNCTIONAL TESTS constitute the content of a special section of sports medicine - functional diagnostics. Functional tests allow you to evaluate the functionality of organs and systems under conditions of additional external influences on the body (physical activity, hypoxia, high or low temperature, etc.)
I.5 Self-assessment questions1. Sports medicine as an integral part of general medicine, its goals and objectives.
2. Dispensary method of monitoring athletes and athletes. The structure of the physical culture and medical dispensary, its tasks.
3. Medical support for physical education and sports in schools, vocational schools, universities, youth sports schools. The division of schoolchildren into medical groups.
4. Medical examination, its goals and objectives.
5. Methods of medical examination, their classification.
II. FOUNDATIONS OF GENERAL PATHOLOGYIII.1 General doctrine of the diseaseGeneral pathology - translated as a general doctrine of diseases (Pathos - disease, logos - teaching), about their most common patterns of occurrence, development and end. For coaches, knowledge of the section of general pathology is associated with the need for a deep understanding of the processes of adaptation of the body to physical and emotional stress in sports, understanding the importance of the principle of individualization of the training process when working with a wide variety of contingents (young athletes and members of the “Health” group, healthy and sick, etc.). etc.), prevention of overvoltage conditions, etc.
A pathological process is a combination of pathological and protective-adaptive reactions in damaged tissues, organs or systems in response to a damaging effect. The simplest forms of pathological processes are called pathological reactions. For example, when a foreign body enters the eye, a lacrimation reaction occurs. Sneezing, coughing are examples of pathological reactions of a protective nature, etc.
A pathological condition is either a slowly developing pathological process, or one of the stages of a pathological process, or a consequence of a pathological process. The pathological process can turn into a pathological state. For example, after a muscle tear in an athlete, a scar forms on the muscle (replacement of muscle tissue with connective tissue), which persists for many years. In scar tissue, as in any living tissue, metabolism occurs, collagen and elastic fibers are formed. A scar is a slowly occurring pathological process, i.e. pathological condition. Conversely, a pathological state can turn into a pathological process. For example, the degeneration of birthmarks into a tumor.
When playing sports, various pathological processes and pathological conditions can be observed that cause disturbances in life and represent, in some cases, a danger to the life of an athlete. These include: cardiac arrest, overexertion, acute disorders of vascular regulation (gravitational syncope, orthostatic collapse), shock, knockouts, hypoglycemic conditions, hypoxia, muscle tears and ruptures, etc. Knowledge of the causes and mechanisms of development of pathological conditions and pathological processes allows the coach to ensure their prevention, and, if necessary, provide first aid.
II.2 Definition of concepts: health, illness, their difference and relationshipHealth and disease are two forms of the organism's vital activity and its adaptation to changing environmental conditions with the help of physiological mechanisms existing in the organism. But this life is qualitatively different. Health is a free life, with full adaptability to changing environmental conditions, with the absence of painful manifestations, preservation of working capacity, etc.
According to the World Health Organization, health is complete physical, mental and social well-being and not merely the absence of disease.
Illness is a cramped life, as the body does not adapt well to changing conditions, painful symptoms appear, and working capacity is impaired. In other words, a disease is a violation of the normal functioning of an organism that occurs under the influence of some damaging effect, characterized by a limitation of adaptation to the external environment, the presence of painful changes and a decrease in working capacity. When a disease occurs, physiological processes continue, but physiological regulation acquires a new character: mechanisms aimed at eliminating the disease-causing principle come first. If these reactions are not enough, then the body mobilizes additional regulatory mechanisms. Thus, illness is a dialectical process. On the one hand, processes of destruction are taking place, and on the other, restoration. Some of the reactions that occur in this case in the body are useful, because. are adaptive, others are harmful.
Between health and disease there is a third intermediate state, when the body is not yet sick, but is no longer healthy either. In this intermediate state, the organism can exist for years. The reasons for the formation of the third state are various adverse effects on the body or exogenous hazards. These conditions include:
– change of time and climate zones
- malnutrition
- bad habits
- professional hazards
- psycho-emotional overload
- hormonal changes in the body (menopause, pubertal changes, etc.)
- pregnancy, etc.
In an intermediate state, the impact of additional hazards or pathogenic factors can lead to a breakdown in adaptation, i.e. to illness. The stay of the organism in the third state should be considered as an opportunity for optimizing adaptive mechanisms in order to maintain health. That is, during this period, health-saving measures are needed. Such activities, for example, include vaccination, fortification, health-improving physical culture, good nutrition, sleep, etc.
II.3 The concept of etiologyEtiology - (aitio - cause) the study of the causes and conditions for the occurrence of diseases.
The cause of the disease is called such a factor that causes the disease and gives it specific features, and without which the occurrence of this disease is impossible. For example, the cause of pneumonia is pneumococcus, tuberculosis is Koch's bacillus. By eliminating the cause of the disease, acting on them with specific drugs, you can achieve recovery. But not always the causative factor causes the disease. For example, during an influenza epidemic, the virus enters the body of almost every person, but not everyone gets sick. That is, the cause alone may or may not cause a disease. Often, the onset of a disease can be put in connection with the influence of not one, but several factors. For example, influenza is promoted by cold (cold), fatigue, negative emotions, malnutrition. Thus, in addition to the cause of the disease, the human body is influenced by factors that contribute to the disease or, conversely, prevent its development. Such factors are called conditions for the onset of the disease. The differences in the causes and conditions of the onset of the disease are:
1) the reason is one, but the conditions are diverse,
2) the reason is obligatory, and the conditions may or may not be,
3) the cause determines the specificity of the disease.
The causes of diseases are factors of the external and internal environment. External (exogenous) factors are divided into:
Physical - factors of a mechanical nature, temperature factors, radiant energy, electric current, low and high atmospheric pressure, etc.
- Chemical - acids, alkalis, poisons of organic and inorganic origin, chemical warfare agents (mustard gas, phosgene, tabun, soman, sarin, etc.), alcohol, nicotine, drugs - cause burns, poisoning
- Nutritional - nutritional factors (malnutrition, overeating), lack of essential nutrients (including vitamins), can cause illness
- Mental - this is primarily excessive negative emotions that can lead to the development of emotiogenic diseases (neurosis, myocardial infarction, stomach ulcers, etc.)
- Social - these are wars, epidemics, famine, unemployment, hypokinesia and hyperkinesia and other influences caused by society and human labor activity.
Hypokinesia is one of the consequences of scientific and technological progress. In translation, the word means a decrease in human motor activity. Automation of production, the development of vehicles, the media (cinema, television) determine the fact that motor activity modern man less than people of the last century. Hypokinesia is a global social problem that affects the entire population of civilized countries. It is considered one of the reasons for the growth of diseases of the cardiovascular system.
Hyperkinesia - excessive physical activity, the use of excessive physical activity, i.e. those that exceed the functional capabilities of the body. Hyperkinesia occurs during irrational physical culture and sports, when excessive loads are the causes of a number of specific diseases associated with physical overstrain.
Internal (endogenous) etiological factors include:
1. constitution
2. heredity